The Connection Between Obesity, Diabetes, and Alzheimer’s
Recent research has shed light on the intricate relationships between obesity, diabetes, and Alzheimer’s disease. These conditions, once thought to be separate health issues, are now understood to be closely interconnected, with each potentially influencing the development and progression of the others.
Obesity and Its Impact
Obesity, characterized by excess body fat, is increasingly recognized as a risk factor for both diabetes and Alzheimer’s disease. A study published in 2025 found that individuals who are overweight or obese in middle age may be more likely to experience cognitive decline and dementia later in life[8]. This connection is particularly strong among older adults.
The Link to Diabetes
Type 2 diabetes, often associated with obesity, is well-known for its effects on blood sugar levels. However, its impact extends beyond just affecting the body’s ability to process glucose. Insulin resistance, a hallmark of Type 2 diabetes, may also play a role in brain health[1].
When the body becomes resistant to insulin, it produces more of this hormone to manage blood sugar. Unfortunately, excess insulin can interfere with the brain’s ability to clear away certain proteins associated with Alzheimer’s disease, potentially contributing to the formation of harmful amyloid clumps[2].
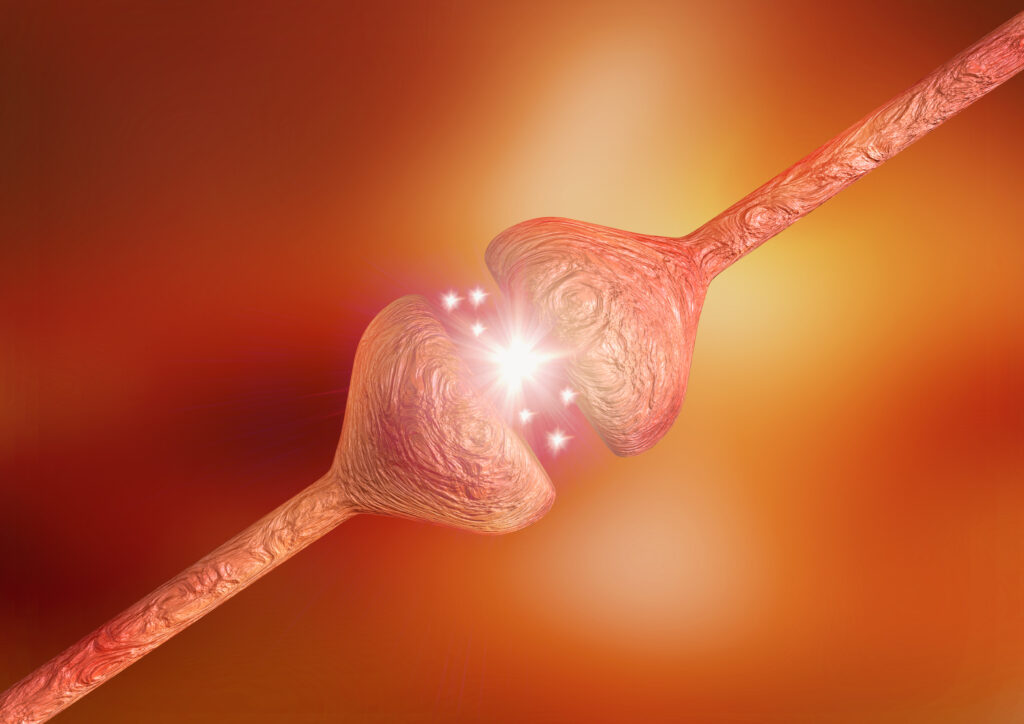
The Alzheimer’s Connection
Alzheimer’s disease, a progressive brain disorder affecting memory and cognitive function, has been increasingly linked to metabolic issues like obesity and diabetes. Some researchers now refer to Alzheimer’s as “Type 3 diabetes,” highlighting the connection between insulin resistance in the brain and cognitive decline[1].
The brain relies heavily on proper insulin function for glucose metabolism. When this process is disrupted, it can lead to neuronal damage and cognitive impairment. This insulin resistance in the brain mirrors what happens in other parts of the body in Type 2 diabetes[1][4].
Shared Risk Factors
Obesity, diabetes, and Alzheimer’s share several risk factors, including:
1. Inflammation: Excess body fat can lead to chronic inflammation, which is associated with both diabetes and Alzheimer’s disease[2].
2. Vascular health: Conditions like high blood pressure, often seen in obesity and diabetes, can affect brain health and increase the risk of dementia[2].
3. Genetic factors: Certain genes, such as APOE ε4, are associated with an increased risk of both Alzheimer’s and metabolic disorders[3].
Prevention and Management
Understanding these connections offers new opportunities for prevention and management:
1. Maintain a healthy weight: Keeping body weight in check can reduce the risk of both diabetes and cognitive decline[2][8].
2. Regular exercise: Physical activity helps manage weight, improve insulin sensitivity, and promote brain health[1].
3. Balanced diet: A diet rich in fruits, vegetables, and whole grains can help maintain healthy blood sugar levels and support brain function[1].
4. Regular check-ups: Early detection and management of conditions like diabetes can potentially reduce the risk of cognitive decline[4].
5. Cognitive stimulation: Engaging in mentally stimulating activities may help maintain brain health, especially for those at higher risk due to obesity or diabetes[1].
Conclusion
The connections between obesity, diabetes, and Alzheimer’s disease underscore the importance of a holistic approach to health. By addressing these conditions together, healthcare providers and individuals can work towards better overall health outcomes and potentially reduce the risk of cognitive decline.
As research in this area continues, it’s becoming increasingly clear that maintaining a healthy weight, managing blood sugar levels, and adopting a brain-healthy lifestyle are crucial steps in protecting both body and min