Zinc deficiency is a genuine, modifiable risk factor for cognitive decline and dementia, and if you or someone you care for is over 65, it deserves your attention. A 2025 retrospective cohort study published in Frontiers in Nutrition found a clear dose-response relationship between zinc deficiency and new-onset dementia, meaning the lower the zinc levels, the higher the risk. This matters because roughly 17 percent of the global population is at risk for inadequate zinc intake, and older adults are particularly vulnerable due to reduced absorption, chronic disease, and medications that interfere with zinc metabolism. The good news is that unlike genetic risk factors, zinc status is something you can actually do something about. Consider a 72-year-old woman who has been eating less over the past few years, relies heavily on toast and tea, and has noticed her sense of taste fading.
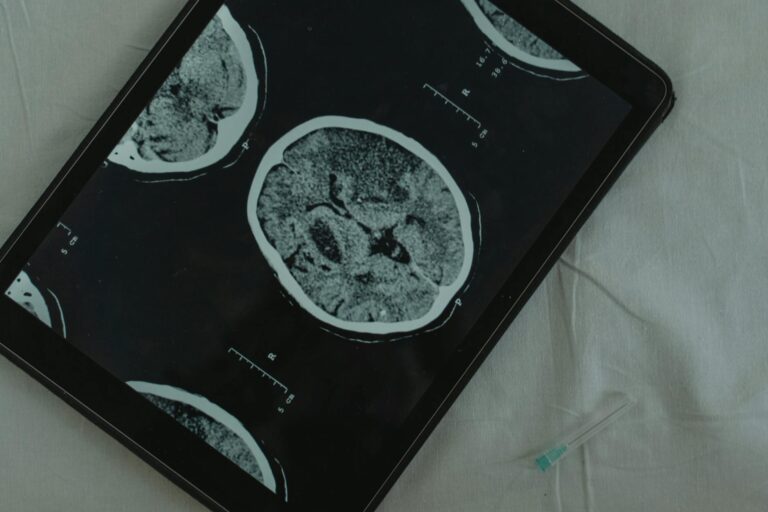
Her doctor attributes the memory lapses to normal aging. But a simple blood test reveals her serum zinc is well below the normal range. This is not an unusual scenario. Zinc is highly concentrated in the hippocampus, the brain region most critical for learning and memory, and when levels drop, the downstream effects on cognition can be significant. This article covers how zinc supports brain function, what the research actually shows about its connection to Alzheimer’s disease, why supplementation is not as straightforward as it sounds, and how to get the right amount without overdoing it.
Table of Contents
- How Does Zinc Deficiency Contribute to Cognitive Decline?
- What the Research Shows About Zinc and Alzheimer’s Disease
- Who Is Most at Risk for Zinc Deficiency?
- How Much Zinc Do You Actually Need?
- Why Zinc Supplementation Is Not a Simple Fix for Dementia
- Getting Tested for Zinc Deficiency
- Where the Science Is Headed
- Conclusion
- Frequently Asked Questions
How Does Zinc Deficiency Contribute to Cognitive Decline?
Zinc is not just another mineral on a nutrition label. In the brain, it plays essential roles in neurotransmission, synaptic plasticity, and neurogenesis — the very processes that underlie your ability to form memories, learn new information, and think clearly. According to research published in the journal Biomolecules, zinc modulates the activity of NMDA receptors and other signaling pathways that keep neurons communicating properly. When zinc levels fall, these processes degrade. Serum zinc concentration gradually decreases with age, and multiple studies published in the International Journal of Molecular Sciences have found that this decline correlates with cognitive impairment and memory problems. What makes zinc deficiency particularly insidious is that its symptoms overlap with what many people write off as normal aging.
Loss of taste and smell, poor wound healing, fatigue, and thinking or reasoning difficulties can all stem from inadequate zinc, according to the NIH Office of Dietary Supplements. A person might spend years attributing these problems to getting older before anyone thinks to check their mineral status. Compare this with something like vitamin B12 deficiency, which doctors screen for more routinely in older adults — zinc rarely gets the same attention, even though the cognitive consequences can be just as real. The World health Organization recognizes zinc deficiency as a significant contributor to the global disease burden, affecting up to two billion people worldwide. In wealthier countries, the problem tends to cluster among older adults, people with gastrointestinal disorders, vegetarians, and those on certain medications like proton pump inhibitors or diuretics. These are large populations, and the overlap with those already at elevated risk for dementia is substantial.

What the Research Shows About Zinc and Alzheimer’s Disease
The connection between zinc and Alzheimer’s disease has moved well beyond speculation. Animal studies published in the Journal of Neuroscience have demonstrated that zinc deficiency worsens Alzheimer’s progression through enhanced NLRP3-driven neuroinflammation — essentially, low zinc ramps up the kind of chronic brain inflammation that accelerates neuronal damage. A 2025 animal study published in Scientific Reports showed that zinc aspartate supplementation produced anti-inflammatory effects and measurable cognitive improvements in rats with Alzheimer’s-modeled disease. These are not fringe findings. They come from established journals and fit within a growing body of evidence.
On the human side, a comprehensive review of nutritional supplements in Alzheimer’s disease conducted from July 2024 to January 2025 noted improvements in cognition following dietary zinc supplementation across several clinical trials. Zinc supplementation has been associated with reduced risk and slower cognitive decline in people with Alzheimer’s disease and mild cognitive impairment, according to research in Biomolecules. However, the relationship is not as simple as “more zinc, less dementia.” The same body of research makes an important caveat clear: both zinc deficiency and excess are associated with cognitive decline. Zinc can exert neuroprotective effects at appropriate levels but becomes neurotoxic at high levels, and may actually promote the formation of amyloid plaques — the hallmark protein deposits found in Alzheimer’s brains. This means that someone who reads a headline about zinc and dementia and starts taking large doses could theoretically make things worse. The therapeutic window matters enormously, and this is a case where more is decidedly not better.
Who Is Most at Risk for Zinc Deficiency?
Older adults carry the highest risk for several compounding reasons. The NIH Office of Dietary supplements notes that aging brings reduced absorption capacity, disease states that alter how the body uses zinc, and increased reliance on medications that decrease zinc bioavailability. A person taking a proton pump inhibitor for acid reflux, a diuretic for blood pressure, and eating smaller meals due to reduced appetite could be hit from three directions at once. Vegetarians and vegans face a distinct challenge. The best dietary sources of zinc are animal-based: oysters contain more zinc per serving than any other food, followed by beef, crab, and lobster.
Plant-based sources like pumpkin seeds, cashews, chickpeas, and lentils do contain zinc, but they also contain phytates — compounds that bind to zinc and significantly lower absorption, as noted by the Harvard School of Public Health. A vegetarian might technically meet the recommended daily allowance on paper while absorbing substantially less in practice. This does not mean a plant-based diet inevitably leads to deficiency, but it does mean vegetarian older adults should pay closer attention to their zinc status. People with gastrointestinal conditions such as Crohn’s disease, ulcerative colitis, or celiac disease are also at elevated risk due to malabsorption. The same goes for people with chronic kidney disease, heavy alcohol use, or sickle cell disease. If you are caring for someone with dementia who also has one of these conditions, zinc deficiency is worth discussing with their medical team, because addressing it could be one of the few interventions that might slow the trajectory.

How Much Zinc Do You Actually Need?
The recommended dietary allowance for zinc, according to the Mayo Clinic, is 11 milligrams per day for adult men and 8 milligrams per day for adult women. The tolerable upper intake level is 40 milligrams per day. That gap between the RDA and the upper limit might seem like plenty of room, but it narrows quickly when you consider that some over-the-counter zinc supplements contain 50 milligrams per tablet, and zinc is also present in many multivitamins and fortified foods. The tradeoff with supplementation is real. At appropriate doses, zinc supports immune function, wound healing, and — as the research increasingly suggests — cognitive health. But chronic intake above 40 milligrams per day can cause copper deficiency, which ironically leads to its own set of neurological problems including numbness, weakness, and difficulty walking. High-dose zinc can also cause nausea, vomiting, and diarrhea, which in an older adult can lead to dehydration and further nutritional problems.
Compare this with something like vitamin D supplementation, where the margin of safety is relatively wider — zinc requires more precision. For most people, food-first is the safer approach. Three ounces of beef provides about 5 milligrams of zinc. A quarter cup of pumpkin seeds provides roughly 2.5 milligrams. A serving of chickpeas adds another 1.3 milligrams. Getting to 8 or 11 milligrams through diet alone is feasible for people who eat a varied diet, though supplementation in the range of 8 to 15 milligrams may be reasonable for those whose intake consistently falls short. Any supplementation decision for someone with cognitive decline should involve their physician, especially because zinc interacts with several common medications.
Why Zinc Supplementation Is Not a Simple Fix for Dementia
Despite promising research, no one should treat zinc as a proven treatment or prevention for Alzheimer’s disease. The evidence so far is suggestive and growing, but it has not yet crossed the threshold that would make clinical guidelines recommend zinc supplementation specifically for dementia prevention. A 24-month, multicentre, randomized, double-blind, placebo-controlled phase II trial has been planned to evaluate zinc sulfate’s efficacy and safety in patients with mild cognitive impairment, according to a study protocol published in Biomolecules. Until trials like this report results, recommendations remain cautious. There is also the issue of individual variation. Two people with the same serum zinc level might respond very differently to supplementation depending on their genetics, their overall nutritional status, the presence of other deficiencies, and the specific form of zinc they take.
Zinc sulfate, zinc gluconate, zinc picolinate, and zinc aspartate all have different absorption profiles. The 2025 animal study that showed cognitive improvements used zinc aspartate specifically, and it is not clear whether those results would replicate with other forms. A final limitation worth stating plainly: most of the strongest evidence comes from animal models. Human observational studies show correlations between zinc levels and cognitive outcomes, but correlation does not prove causation. People with zinc deficiency often have other nutritional deficiencies, lower socioeconomic status, or more chronic disease — all of which independently increase dementia risk. The 2025 Frontiers in Nutrition study is notable because it identified zinc deficiency as an independent risk factor after adjusting for these confounders, but it remains a single study. Replication matters.

Getting Tested for Zinc Deficiency
If you are concerned about zinc status — either your own or that of someone you are caring for — the first step is a serum zinc test, which is a simple blood draw available through most primary care physicians. The normal range is typically between 60 and 120 micrograms per deciliter, though reference ranges vary slightly between laboratories.
It is worth noting that serum zinc is not a perfect measure because only about 0.1 percent of the body’s zinc circulates in the blood, but it is the most widely available and clinically accepted test. Ask for zinc testing if there are symptoms that suggest deficiency: persistent changes in taste or smell, unexplained skin rashes, slow wound healing, frequent infections, or cognitive changes that seem out of proportion to age. For someone already diagnosed with mild cognitive impairment or early Alzheimer’s, checking zinc levels is a low-cost, low-risk step that could identify a treatable contributing factor.
Where the Science Is Headed
The next few years should bring substantially more clarity to the zinc-cognition question. The planned 24-month randomized controlled trial on zinc sulfate in mild cognitive impairment will be one of the most rigorous tests of the hypothesis to date. If it shows a meaningful benefit, it could shift clinical practice toward routine zinc screening in people with early cognitive symptoms — a change that would be both inexpensive and easy to implement.
Researchers are also exploring how zinc interacts with other nutrients in the context of brain health, including selenium, copper, and omega-3 fatty acids. The emerging picture suggests that single-nutrient interventions may be less effective than addressing the broader nutritional profile, which aligns with what we know about how dementia develops through multiple overlapping pathways rather than a single cause. For caregivers and families navigating a dementia diagnosis, the practical takeaway is that nutrition — zinc included — belongs in the conversation alongside medication, exercise, and cognitive engagement.
Conclusion
Zinc deficiency is increasingly recognized as a modifiable risk factor for cognitive decline and dementia. The evidence linking low zinc levels to impaired neurotransmission, increased neuroinflammation, and accelerated Alzheimer’s progression is substantial and growing. Older adults are disproportionately affected due to reduced absorption, dietary changes, and medication interactions. Getting enough zinc through diet — or through careful, physician-guided supplementation — is a reasonable, evidence-based step for supporting brain health.
At the same time, zinc is not a miracle cure, and taking too much carries its own risks, including copper deficiency and potentially worsening amyloid pathology. The right approach is measured: know the RDA (11 milligrams for men, 8 milligrams for women), prioritize zinc-rich foods, get tested if symptoms suggest a deficiency, and talk to a doctor before supplementing. As larger clinical trials report results over the coming years, we will have a clearer picture of exactly how much zinc supplementation can do for cognitive health. In the meantime, making sure you are not deficient is one of the simplest and most actionable things you can do for your brain.
Frequently Asked Questions
Can zinc supplements reverse dementia?
No supplement has been proven to reverse dementia. However, zinc supplementation has been associated with reduced risk and slower cognitive decline in people with Alzheimer’s disease and mild cognitive impairment. Correcting a deficiency may help optimize brain function, but it is not a cure.
How do I know if I am zinc deficient?
A serum zinc blood test is the most common method. Symptoms of deficiency include loss of taste or smell, slow wound healing, frequent infections, skin lesions, hair loss, and problems with thinking and memory. If you have several of these symptoms, ask your doctor for testing.
Is it safe to take zinc supplements long-term?
At doses within the recommended daily allowance (8 to 11 milligrams), long-term zinc supplementation is generally considered safe for most adults. However, the tolerable upper intake level is 40 milligrams per day, and chronic high-dose use can cause copper deficiency and other adverse effects. Always consult a physician before starting long-term supplementation.
Are vegetarians more likely to be zinc deficient?
Vegetarians and vegans face a higher risk because the best zinc sources are animal-based (oysters, beef, crab), and plant-based sources contain phytates that reduce zinc absorption. Soaking, sprouting, or fermenting grains and legumes can help reduce phytate content and improve zinc availability.
Does zinc interact with medications?
Yes. Zinc can interact with antibiotics (tetracyclines and quinolones), diuretics, and penicillamine. Proton pump inhibitors and certain diuretics can also reduce zinc absorption over time. If you take any of these medications regularly, discuss zinc supplementation with your healthcare provider.
What is the best food source of zinc?
Oysters contain more zinc per serving than any other food — a single three-ounce serving provides far more than the daily requirement. Other strong sources include beef, crab, lobster, pumpkin seeds, cashews, chickpeas, and lentils. A varied diet that includes some animal protein typically provides adequate zinc.