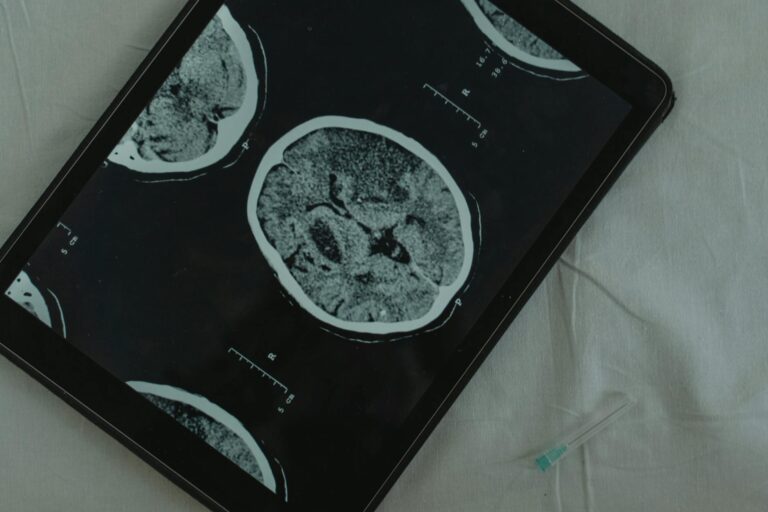
CoQ10 shows real promise as a brain supplement, but the honest answer is that the science remains split. Out of eight human clinical trials examined in a comprehensive review published in Nutrients in September 2025, four showed a beneficial effect on cognition and two demonstrated increased cerebral blood flow. The other trials reported no cognitive benefit at all. That is not a ringing endorsement, but it is not a dismissal either. For someone watching a parent struggle with early cognitive decline and wondering whether CoQ10 belongs in the daily regimen, the picture is genuinely complicated, and the complications matter more than the marketing claims on the bottle. The reason CoQ10 attracts so much attention from brain health researchers is straightforward.
Your brain is an energy hog. It accounts for roughly two percent of your body weight but consumes about twenty percent of your energy. That energy comes from mitochondria, and CoQ10 is an essential component of the mitochondrial oxidative phosphorylation system that produces ATP, the molecule your cells use as fuel. CoQ10 also functions as an antioxidant, scavenging free radicals directly and regenerating other antioxidants indirectly. When CoQ10 levels decline with age, mitochondrial function follows, and the brain feels it. This article walks through what the clinical trials actually found, where animal research diverges from human results, why the blood-brain barrier is the elephant in the room, how different CoQ10 formulations compare, and what practical decisions a caregiver or patient can make with the evidence as it stands today.
Table of Contents
- How Does CoQ10 Power Mitochondrial Energy in the Brain?
- What Do the Human Clinical Trials Actually Show?
- The Blood-Brain Barrier Problem
- Ubiquinol Versus Ubiquinone and Why Formulation Matters More Than You Think
- Dosage Ranges and the Safety Question
- CoQ10 and Fatigue, a Related Benefit for Caregivers and Patients
- What Comes Next in CoQ10 Brain Research
- Conclusion
- Frequently Asked Questions
How Does CoQ10 Power Mitochondrial Energy in the Brain?
CoQ10, also known as coenzyme Q10 or ubiquinone, serves as an electron transporter in the mitochondrial energy production chain. Without adequate CoQ10, the chain slows down, ATP production drops, and cells that depend heavily on energy, particularly neurons, begin to struggle. This is not a theoretical concern. Research in mouse models has shown that age-associated declines in mitochondrial function, including reduced oxygen consumption rate, lower cytochrome c oxidase activity, and decreased mitochondrial CoQ levels, begin as early as twelve to fifteen months of age in male mouse brains. In human terms, that is roughly equivalent to middle age. The decline is not just about energy. When mitochondria underperform, they produce more reactive oxygen species, the unstable molecules that damage DNA, proteins, and cell membranes.
CoQ10 combats this on two fronts: it keeps energy production efficient, and it neutralizes the oxidative byproducts when efficiency slips. In rat models of Alzheimer’s disease, CoQ10 therapy improved memory, retention, and learning, with substantial decreases in oxidative stress and measurable increases in ATP levels in the cerebral cortex and hippocampus. That is the mechanism working exactly as you would hope. But here is where the comparison between mice and humans matters. In those same mouse studies, age-associated declines in mitochondrial function and CoQ levels were completely rescued by exogenous water-soluble CoQ10 administration. Oral CoQ10 has been shown to increase brain and brain mitochondrial concentrations in animals and to exert neuroprotective effects. The question is whether the same thing happens in a human brain, and the answer, as we will see, is far less certain.

What Do the Human Clinical Trials Actually Show?
The most useful summary of human evidence comes from the September 2025 review in Nutrients, which examined all available clinical data on CoQ10 and cognition. Among the eight human trials reviewed, two were conducted in healthy subjects and six in people with existing disease states. The results split roughly down the middle. Four trials showed cognitive benefit, two showed increased cerebral blood flow, and several showed no benefit at all. The inconsistencies are attributed to differing testing procedures, inconsistent cognitive assessments across studies, and varying bioavailability of different CoQ10 preparations. The most encouraging single trial involved eighty patients with early Parkinson’s disease who received 300, 600, or 1,200 milligrams per day in a randomized, placebo-controlled design. The supplementation was well-tolerated and associated with slower deterioration of cognitive functions compared to placebo.
However, the story changes with Alzheimer’s disease. A clinical trial using 400 milligrams per day for sixteen weeks in Alzheimer’s patients found no improvement in oxidative stress markers or neurodegeneration biomarkers. Small clinical trials in Huntington’s disease and ALS have also failed to show benefit. The warning here is important for families making decisions. A result in early Parkinson’s does not automatically transfer to Alzheimer’s or other forms of dementia. These are different diseases with different mechanisms of neurodegeneration, even if mitochondrial dysfunction plays some role in all of them. If someone tells you CoQ10 is proven to help with dementia broadly, they are overstating the evidence.
The Blood-Brain Barrier Problem
This is the issue that rarely makes it onto supplement labels. No clinical study has unambiguously shown that orally administered CoQ10 directly crosses the blood-brain barrier and accesses the human brain. The blood-brain barrier is a selective membrane that protects the brain from toxins and pathogens, but it also blocks many potentially beneficial compounds. CoQ10 is a large, fat-soluble molecule, and getting it past this barrier in meaningful concentrations is a genuine challenge. There is a sliver of encouraging data. One study by Mitsui and colleagues reported increased ubiquinol levels in cerebrospinal fluid of patients with multiple system atrophy after oral supplementation. The reduced form of CoQ10, ubiquinol, may have some ability to access the blood-brain barrier.
But cerebrospinal fluid access is not the same as brain parenchyma access. The CSF bathes the brain, but reaching the neurons embedded in brain tissue is a different and more demanding task. This is the fundamental tension in CoQ10 brain research. The animal data is promising because you can measure CoQ10 directly in brain tissue after supplementation. In humans, you are largely guessing. The benefits observed in some clinical trials might come from CoQ10’s effects on vascular health, systemic inflammation, or energy metabolism elsewhere in the body, rather than from direct action in the brain. Until this question is resolved, every claim about CoQ10 and brain health carries an asterisk.
Ubiquinol Versus Ubiquinone and Why Formulation Matters More Than You Think
Walk into any supplement aisle and you will find CoQ10 sold in two forms: ubiquinone, the oxidized form, and ubiquinol, the reduced form. Ubiquinol is typically marketed as superior because it is the active antioxidant form and has been shown to have roughly double the bioavailability of standard ubiquinone. But the full story is more nuanced. Research has shown that ubiquinol’s bioavailability was only about 52 percent that of thermally crystal-modified ubiquinone, a processed form of the supposedly inferior version. In other words, how CoQ10 is manufactured and formulated can matter more than whether it is ubiquinol or ubiquinone. There is another wrinkle.
Under simulated stomach and intestinal conditions, supplemental ubiquinol is largely oxidized to ubiquinone before it even enters intestinal cells. So the premium you pay for ubiquinol may be partially undone by your own digestive system. This does not mean ubiquinol supplements are worthless, but it does mean the marketing distinction between the two forms is overblown. What matters more is the delivery technology, whether the product uses solubilized softgels, crystal-modified preparations, or other absorption-enhancing techniques. For practical purposes, CoQ10 is fat-soluble and best absorbed when taken with a fat-containing meal. If you are taking CoQ10 on an empty stomach or with just water, you are likely wasting a significant portion of it regardless of which form you chose.
Dosage Ranges and the Safety Question
Clinical study doses have ranged enormously, from 50 milligrams per day to 1,200 milligrams per day in standard trials, and up to 3,000 milligrams per day in some neurodegenerative disease research. Standard supplementation typically falls in the 60 to 500 milligram range. For the Parkinson’s trial that showed cognitive benefit, the highest dose used was 1,200 milligrams per day. The Alzheimer’s trial that showed no benefit used 400 milligrams per day for sixteen weeks. Whether the Alzheimer’s result would have differed at a higher dose or longer duration is unknown. CoQ10 is considered safe and well-tolerated even at high doses of 1,200 to 2,400 milligrams per day. Side effects, when they occur, tend to be mild gastrointestinal symptoms.
However, safety is not the same as efficacy. A supplement can be perfectly safe and do nothing useful. The limitation that families need to understand is that we still cannot say with confidence whether CoQ10 reverses or meaningfully slows functional decline of mitochondria in the human brain. The animal evidence suggests it can. The human evidence is not there yet. One important caution: CoQ10 can interact with blood thinners like warfarin, potentially reducing their effectiveness. Anyone on anticoagulant therapy should consult their physician before starting CoQ10 supplementation, particularly at higher doses.

CoQ10 and Fatigue, a Related Benefit for Caregivers and Patients
Beyond cognition, CoQ10 has a more consistent evidence base for reducing fatigue. A systematic review and meta-analysis of randomized controlled trials found that CoQ10 supplementation shows statistically significant effects in reducing fatigue symptoms and is considered effective and safe for this purpose. For dementia caregivers experiencing chronic exhaustion, or for patients in early cognitive decline who report persistent tiredness, this may be a practical reason to consider CoQ10 even if the cognitive benefits remain uncertain.
Fatigue and cognitive function are not entirely separate concerns. Chronic fatigue impairs attention, memory consolidation, and executive function. If CoQ10 helps a person feel less physically drained, the downstream effects on mental sharpness could be real, even if the mechanism is indirect rather than through direct brain action.
What Comes Next in CoQ10 Brain Research
The field is not standing still. A 90-day randomized controlled trial evaluating ubiquinol’s cognitive effects in healthy elderly participants was designed, with results expected around 2025. Studies like this one, which focus on healthy aging rather than established disease, may provide clearer answers about whether CoQ10 can protect cognitive function before significant decline sets in, which is arguably the more useful question for most people.
The blood-brain barrier problem is also driving research into novel delivery systems, including nanoparticle formulations and water-soluble CoQ10 preparations that showed such striking results in animal models. If researchers can demonstrate that a specific formulation reliably increases CoQ10 concentrations in human brain tissue, the clinical trial landscape could shift substantially. Until then, CoQ10 for brain health remains a reasonable bet with an incomplete evidence base, not a proven therapy but not a baseless one either.
Conclusion
CoQ10 is a genuinely important molecule for brain energy metabolism, and the biological rationale for supplementation is sound. Your brain needs enormous amounts of ATP, CoQ10 helps produce it, and levels decline with age. Animal studies consistently show that CoQ10 supplementation can restore mitochondrial function, reduce oxidative stress, and improve memory. But the leap from mouse brains to human brains has not been cleanly made.
About half of human trials show cognitive benefit, and the fundamental question of whether oral CoQ10 actually reaches the human brain in meaningful amounts remains unanswered. For families navigating dementia or cognitive decline, CoQ10 is worth discussing with a physician, particularly given its strong safety profile and potential benefits for fatigue. It should not replace established treatments or lifestyle interventions like exercise, sleep optimization, and social engagement, which have more robust evidence for cognitive protection. Take it with a fat-containing meal, do not overpay for ubiquinol based on marketing alone, and keep expectations grounded. The science may eventually catch up to the promise, but it has not arrived there yet.
Frequently Asked Questions
What dose of CoQ10 should I take for brain health?
There is no established optimal dose for cognitive benefit. Clinical trials have used anywhere from 50 to 1,200 milligrams per day. Standard supplementation ranges from 60 to 500 milligrams daily. The Parkinson’s trial showing cognitive benefit used up to 1,200 milligrams per day, while an Alzheimer’s trial at 400 milligrams showed no effect. Start with a moderate dose and discuss higher amounts with your doctor.
Is ubiquinol better than ubiquinone for the brain?
Not necessarily. While ubiquinol has roughly double the bioavailability of standard ubiquinone, thermally crystal-modified ubiquinone actually outperformed ubiquinol in absorption studies. Additionally, supplemental ubiquinol is largely oxidized to ubiquinone in the digestive tract before absorption. The formulation and delivery technology matter more than the form itself.
Does CoQ10 cross the blood-brain barrier?
No clinical study has unambiguously demonstrated that orally administered CoQ10 crosses the blood-brain barrier and reaches human brain tissue. One study found increased ubiquinol in cerebrospinal fluid after supplementation, but cerebrospinal fluid access does not confirm penetration into brain tissue itself. This remains a major open question.
Can CoQ10 help with Alzheimer’s disease?
The evidence is not encouraging for established Alzheimer’s. A clinical trial using 400 milligrams per day for sixteen weeks in Alzheimer’s patients found no improvement in oxidative stress markers or neurodegeneration biomarkers. Animal models show benefits, but these have not translated to human Alzheimer’s trials so far.
Is CoQ10 safe to take long-term?
CoQ10 is considered safe and well-tolerated even at high doses of 1,200 to 2,400 milligrams per day. Mild gastrointestinal symptoms are the most common side effect. However, CoQ10 can interact with blood thinners like warfarin, so anyone on anticoagulant therapy should consult their doctor first.
When should I take CoQ10 for best absorption?
CoQ10 is fat-soluble and best absorbed when taken with a meal containing dietary fat. Taking it on an empty stomach significantly reduces absorption regardless of the formulation you use.