Amyloid antibody treatments represent one of the most significant developments in Alzheimer’s disease research in decades, offering new hope for millions of patients and families affected by this devastating condition. After years of clinical failures targeting amyloid plaques in the brain, recent breakthroughs have demonstrated that removing these protein deposits can meaningfully slow cognitive decline in people with early-stage Alzheimer’s disease. This shift from skepticism to cautious optimism marks a turning point in how the medical community approaches dementia treatment. The question of why amyloid antibody treatments show promise goes beyond simple plaque removal.
These therapies validate a fundamental theory about Alzheimer’s pathology while opening doors to earlier intervention and combination approaches that could prove even more effective. For patients and caregivers navigating a diagnosis, understanding these treatments means grasping both their potential benefits and their limitations””knowledge that can inform treatment decisions and set realistic expectations. This article examines the science behind amyloid-targeting antibodies, reviews the clinical evidence supporting their use, discusses who might benefit most from these therapies, and addresses practical considerations for patients considering treatment. By the end, readers will have a comprehensive understanding of where these treatments fit in the current landscape of Alzheimer’s care and what the future might hold for this approach.
Table of Contents
- What Are Amyloid Antibody Treatments and How Do They Work?
- Clinical Evidence Supporting Amyloid-Targeting Therapies
- Understanding the Benefits and Risks of Amyloid Antibodies
- Who Are the Best Candidates for Amyloid Antibody Treatment?
- Challenges and Limitations Facing Amyloid-Targeting Approaches
- Future Directions in Amyloid-Based Alzheimer’s Research
- How to Prepare
- How to Apply This
- Expert Tips
- Conclusion
- Frequently Asked Questions
What Are Amyloid Antibody Treatments and How Do They Work?
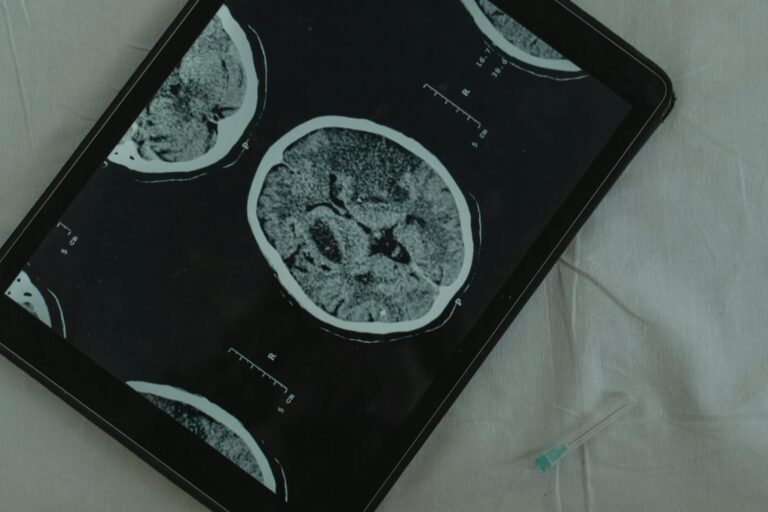
Amyloid antibody treatments are a class of immunotherapy drugs designed to target and remove beta-amyloid protein from the brain. Beta-amyloid naturally occurs in healthy brains, but in Alzheimer’s disease, these proteins misfold and clump together to form plaques that accumulate between neurons. These plaques disrupt cell communication, trigger inflammation, and contribute to the progressive brain damage characteristic of Alzheimer’s. Amyloid antibodies are laboratory-engineered proteins that bind specifically to different forms of beta-amyloid, flagging them for removal by the body’s immune system.
The mechanism works through several pathways depending on the specific antibody design. some antibodies target soluble amyloid oligomers””small, toxic clusters thought to cause early neuronal damage””while others focus on removing established plaques from brain tissue. When these antibodies bind to amyloid, they recruit microglial cells, the brain’s resident immune cells, which then engulf and clear the protein deposits. This process, visible on PET imaging scans, shows dramatic reductions in amyloid burden over months of treatment. Three key concepts define how these treatments function:.
- **Selective targeting**: Unlike broad immunosuppressants, amyloid antibodies are highly specific, binding only to particular configurations of beta-amyloid while leaving healthy proteins untouched.
- **Immune activation**: The antibodies essentially teach the immune system to recognize amyloid as foreign material requiring removal, amplifying the brain’s natural clearance mechanisms.
- **Continuous administration**: Because amyloid continues forming, these treatments require ongoing infusions, typically every two to four weeks, to maintain reduced plaque levels.
Clinical Evidence Supporting Amyloid-Targeting Therapies
The clinical evidence for amyloid antibody treatments has evolved substantially since early disappointing trials. Lecanemab, approved by the FDA in 2023, demonstrated in its Phase 3 CLARITY AD trial that treated patients experienced 27% less cognitive decline over 18 months compared to those receiving placebo. While this may sound modest, it represents the first time any treatment has shown statistically significant slowing of Alzheimer’s progression in a large, well-designed trial. Donanemab, another amyloid antibody, showed even more pronounced effects in certain patient populations, with some participants experiencing up to 35% slowing of decline.
These results become more meaningful when examining the data closely. Patients who achieved complete amyloid clearance””measured by PET scans showing plaque levels below the threshold for Alzheimer’s pathology””showed the greatest clinical benefit. In the donanemab trials, participants who cleared their amyloid and were switched to placebo maintained their cognitive gains, suggesting the treatment effect persists even after stopping therapy. This finding challenges earlier assumptions that any benefit would be temporary and supports the hypothesis that removing amyloid addresses an underlying disease mechanism. Important considerations from the clinical data include:.
- **Early-stage focus**: Current approvals are limited to patients with mild cognitive impairment or mild dementia due to Alzheimer’s, with confirmed amyloid pathology via PET scan or cerebrospinal fluid analysis.
- **Biomarker confirmation**: Trials required objective evidence of amyloid accumulation, meaning these treatments are not appropriate for all forms of dementia or cognitive decline.
- **Consistent plaque reduction**: Across multiple trials, amyloid antibodies reduced brain amyloid levels by 60-80% over 12-18 months, providing clear biological evidence of target engagement.
Understanding the Benefits and Risks of Amyloid Antibodies
The benefit-risk calculation for amyloid antibody treatments requires careful consideration of individual circumstances. On the benefit side, slowing cognitive decline by roughly one-quarter to one-third translates to preserving functional abilities longer””maintaining independence in daily activities, retaining the capacity to manage finances, and prolonging the period when meaningful conversations remain possible. For many patients and families, these months or years of preserved function carry immense value, even if the treatment does not stop progression entirely. The most significant risk associated with amyloid antibodies is amyloid-related imaging abnormalities, known as ARIA.
This category includes ARIA-E (edema or fluid accumulation in the brain) and ARIA-H (microhemorrhages or superficial iron deposits). In clinical trials, ARIA occurred in 20-35% of treated patients, though most cases were asymptomatic and detected only through routine MRI monitoring. Symptomatic ARIA, causing headaches, confusion, or visual disturbances, occurred in roughly 3-5% of participants. While most cases resolve with temporary treatment interruption, serious complications including hospitalization and rare fatalities have occurred. Key risk factors and considerations include:.
- **APOE4 gene status**: Patients carrying two copies of the APOE4 gene variant face substantially higher ARIA risk, up to 40-50% in some trials, requiring particularly careful monitoring and informed consent discussions.
- **Anticoagulant use**: Blood thinners may increase the severity of ARIA-related bleeding, complicating treatment for patients requiring anticoagulation for heart conditions or stroke prevention.

Who Are the Best Candidates for Amyloid Antibody Treatment?
Identifying appropriate candidates for amyloid antibody therapy involves multiple clinical, biological, and practical considerations. The clearest candidates are individuals with early symptomatic Alzheimer’s disease””specifically those with mild cognitive impairment or mild dementia””who have biomarker confirmation of amyloid pathology. This typically means a positive amyloid PET scan or cerebrospinal fluid analysis showing elevated beta-amyloid levels. The restriction to early-stage disease reflects trial data showing the greatest benefit in this population, while patients with moderate or advanced dementia showed minimal response in earlier studies. Beyond disease stage, several factors influence candidacy decisions.
Patients must be able to tolerate regular MRI scans for ARIA monitoring, typically required before every other infusion during the initial treatment period. They need access to infusion centers capable of administering these medications and managing potential reactions. Importantly, candidates should have realistic expectations about outcomes””these treatments slow decline rather than restore lost function or stop progression entirely. A thorough discussion between patients, families, and neurologists should weigh potential benefits against risks based on individual health status and values. Practical candidacy considerations include:.
- **Cardiovascular health**: Stable cardiac function is important given infusion requirements and ARIA risks.
- **Support system**: Regular treatment appointments and monitoring require reliable transportation and often caregiver involvement.
- **Cognitive capacity for consent**: Patients should ideally participate in treatment decisions while they retain capacity to understand the benefits, risks, and alternatives.
- **Access considerations**: Geographic proximity to treatment centers and insurance coverage significantly impact whether treatment is feasible.
Challenges and Limitations Facing Amyloid-Targeting Approaches
Despite their promise, amyloid antibody treatments face substantial challenges that temper enthusiasm. The modest effect sizes””27-35% slowing of decline””mean that patients still progress, and distinguishing treatment benefit from placebo effect can be difficult in individual cases. Critics argue that the clinical meaningfulness of these statistical differences remains debatable, particularly given the treatments’ high costs and safety monitoring requirements. Some researchers question whether targeting amyloid addresses the primary driver of Alzheimer’s or merely one contributor among many.
The amyloid hypothesis itself, while supported by genetic evidence and now treatment data, does not fully explain Alzheimer’s pathology. Many individuals with significant amyloid accumulation never develop symptoms, while some Alzheimer’s patients show minimal plaque burden. This discordance suggests that factors beyond amyloid””including tau protein tangles, neuroinflammation, vascular changes, and synaptic dysfunction””play crucial roles in disease progression. Future treatments may need to address multiple pathways simultaneously to achieve more substantial benefits. Practical challenges creating barriers to widespread adoption include:.
- **Cost**: Annual treatment costs exceeding $26,000, plus monitoring expenses, create significant access disparities.
- **Infrastructure**: Many communities lack the specialized imaging, infusion capabilities, and neurological expertise required for safe treatment administration.
- **Diagnosis gaps**: The requirement for biomarker confirmation exposes the inadequacy of current diagnostic pathways, where many patients receive dementia diagnoses without amyloid testing.
- **Monitoring burden**: Frequent MRIs and infusions demand substantial time commitments from patients and healthcare systems.

Future Directions in Amyloid-Based Alzheimer’s Research
Research continues advancing beyond current first-generation amyloid antibodies toward potentially more effective approaches. Scientists are investigating whether treating amyloid accumulation before symptoms appear””in preclinical Alzheimer’s disease””might provide greater benefit by intervening before substantial neurodegeneration occurs. Large prevention trials in genetically at-risk populations are testing whether early amyloid removal can delay or prevent cognitive symptoms entirely, though results will take years to materialize.
Combination therapy strategies represent another promising direction. Researchers are designing trials pairing amyloid antibodies with treatments targeting tau protein, neuroinflammation, or other disease mechanisms. The rationale mirrors successful approaches in cancer and HIV treatment, where attacking disease through multiple pathways proves more effective than single-target therapies. Advances in delivery methods, including subcutaneous injections that patients could administer at home, may also improve treatment accessibility and reduce the burden of frequent infusion center visits.
How to Prepare
- **Obtain comprehensive diagnostic testing** that confirms Alzheimer’s pathology through biomarkers. This typically requires an amyloid PET scan or lumbar puncture for cerebrospinal fluid analysis, in addition to standard cognitive assessments and structural brain imaging. Insurance coverage for these tests varies, so clarify costs beforehand.
- **Undergo APOE genetic testing** to understand your personal ARIA risk profile. While not universally required, knowing your APOE4 status helps inform risk discussions. Some patients decline this information, which is an acceptable choice, but most treatment centers recommend it.
- **Compile a complete medication list** including all prescription drugs, supplements, and over-the-counter products. Pay particular attention to blood thinners, antiplatelet agents, and any medications affecting bleeding risk, as these influence treatment safety.
- **Evaluate your support network** and logistical capacity for ongoing treatment. Consider who will accompany you to infusions, how you will travel to appointments every two to four weeks, and who will monitor for symptoms between visits. Honest assessment prevents treatment interruption due to practical barriers.
- **Prepare questions for your neurologist** about expected benefits in your specific case, how treatment response will be measured, what symptoms should prompt immediate contact, and under what circumstances treatment would be discontinued.
How to Apply This
- **Schedule a consultation with a dementia specialist** at a center experienced with these treatments. General neurologists may not have the infrastructure or expertise for safe administration and monitoring. Academic medical centers and large neurology practices typically offer the most comprehensive programs.
- **Complete the required pre-treatment evaluation** including baseline MRI, cognitive testing, and biomarker confirmation. This establishes comparison points for monitoring treatment response and detecting ARIA early.
- **Develop a monitoring and communication plan** with your treatment team. Understand the MRI schedule, know which symptoms require immediate reporting, and ensure you have direct contact information for your treatment coordinator.
- **Establish realistic milestones** for evaluating whether treatment is working for you. While individual response varies, most patients can assess tolerability within the first few months and preliminary efficacy based on cognitive assessments at 6-12 months.
Expert Tips
- **Start a symptom diary before beginning treatment** to establish your personal baseline. Note daily function, mood, sleep patterns, and any neurological symptoms like headaches or visual changes. This documentation helps distinguish treatment-related effects from normal fluctuation.
- **Advocate for comprehensive genetic counseling** before APOE testing. Learning you carry high-risk genes affects not only treatment decisions but also has implications for family members and insurance coverage that deserve careful consideration.
- **Consider participating in clinical trials** even if standard treatments are available. Trials offer access to next-generation therapies and contribute knowledge that benefits future patients. Ask your neurologist about open studies matching your profile.
- **Prioritize overall brain health** alongside specific treatments. Evidence-based interventions including regular exercise, social engagement, cognitive stimulation, cardiovascular risk management, and quality sleep support brain resilience regardless of whether you pursue amyloid antibody therapy.
- **Connect with patient advocacy organizations** for practical support and current information. Groups like the Alzheimer’s Association maintain resources on treatment access, insurance navigation, and peer support that complement medical care.
Conclusion
Amyloid antibody treatments mark a genuine turning point in Alzheimer’s disease therapy, validating decades of research into amyloid pathology while providing the first disease-modifying options for patients with early-stage illness. The evidence shows these treatments can slow cognitive decline meaningfully, though they do not stop progression or restore lost function. Understanding both the promise and the limitations helps patients and families make informed decisions aligned with their values and circumstances.
The path forward involves continued research into earlier intervention, combination approaches, and improved accessibility. For individuals facing an Alzheimer’s diagnosis today, these treatments offer one tool among many for maintaining quality of life and functional independence. The best outcomes result from comprehensive care that combines appropriate medical treatment with lifestyle optimization, caregiver support, and advance planning. While amyloid antibodies are not a cure, they represent genuine progress toward that ultimate goal and provide hope that continued scientific effort will yield even more effective therapies in the years ahead.
Frequently Asked Questions
How long does it typically take to see results?
Results vary depending on individual circumstances, but most people begin to see meaningful progress within 4-8 weeks of consistent effort. Patience and persistence are key factors in achieving lasting outcomes.
Is this approach suitable for beginners?
Yes, this approach works well for beginners when implemented gradually. Starting with the fundamentals and building up over time leads to better long-term results than trying to do everything at once.
What are the most common mistakes to avoid?
The most common mistakes include rushing the process, skipping foundational steps, and failing to track progress. Taking a methodical approach and learning from both successes and setbacks leads to better outcomes.
How can I measure my progress effectively?
Set specific, measurable goals at the outset and track relevant metrics regularly. Keep a journal or log to document your journey, and periodically review your progress against your initial objectives.
When should I seek professional help?
Consider consulting a professional if you encounter persistent challenges, need specialized expertise, or want to accelerate your progress. Professional guidance can provide valuable insights and help you avoid costly mistakes.
What resources do you recommend for further learning?
Look for reputable sources in the field, including industry publications, expert blogs, and educational courses. Joining communities of practitioners can also provide valuable peer support and knowledge sharing.