No, there is no generic version of lecanemab available, and there will not be one for many years. Lecanemab is sold exclusively under the brand name Leqembi, manufactured by Eisai and Biogen. Because it is a biologic drug — a complex monoclonal antibody — it cannot have a traditional generic equivalent. Instead, it would require a biosimilar, a distinct regulatory category with its own approval pathway.
Given that lecanemab received FDA approval in 2023, U.S. law grants it 12 years of market exclusivity, meaning the earliest a biosimilar could realistically enter the market is around 2035 — and that assumes a manufacturer has already begun development, which none have publicly announced. This matters enormously for families trying to access treatment. At a list price of approximately $26,500 per year, cost is a major barrier for many early Alzheimer’s patients. This article explains why a generic or biosimilar version does not exist, when one might become available, what the current coverage landscape looks like through Medicare and insurance, and what options families can realistically explore today while waiting for the drug’s costs to come down.
Table of Contents
- Why Is There No Generic Lecanemab Available?
- When Could a Biosimilar Lecanemab Become Available?
- What Formulations of Leqembi Currently Exist?
- What Does Leqembi Cost and Who Pays for It?
- What Are the Eligibility and Safety Considerations?
- Are There Any Lower-Cost Alternatives for Dementia Treatment?
- What Should Families Expect in the Coming Years?
- Conclusion
- Frequently Asked Questions
Why Is There No Generic Lecanemab Available?
The word “generic” applies to small-molecule drugs — pills and tablets made from chemical compounds that can be replicated precisely once patents expire. Aspirin, metformin, lisinopril: these all have generics. Lecanemab is a fundamentally different kind of medicine. It is a monoclonal antibody, a large and complex protein engineered to bind to amyloid-beta plaques in the brain. Manufacturing a molecule this large and intricate is not a matter of following a chemical recipe. It requires living cell cultures, highly controlled biological processes, and specialized equipment that cannot simply be copied and sold as a “generic.” What biologics like lecanemab can eventually have are biosimilars — drugs that are highly similar to the original but not identical, developed through their own rigorous clinical and regulatory process.
The FDA evaluates biosimilars under a separate pathway established by the Biologics Price Competition and Innovation Act. To put this in perspective, the first biosimilar of adalimumab (Humira, one of the world’s top-selling biologics) took years to reach patients even after exclusivity ended, faced numerous patent disputes, and required extensive clinical data to demonstrate comparability. Lecanemab is earlier in its life cycle by a decade. Until that biosimilar pathway is available and a manufacturer commits to pursuing it, lecanemab remains a single-source drug with no competition to drive down price. For patients comparing this situation to, say, the rapid appearance of generic Aricept (donepezil) after its patent expired, the difference is stark: donepezil is a small molecule, and generics appeared quickly and cheaply. The same will not happen with lecanemab.

When Could a Biosimilar Lecanemab Become Available?
The exclusivity math is straightforward but sobering. Lecanemab received FDA accelerated approval in January 2023 and traditional approval in July 2023. The 12-year biologic exclusivity clock runs from the approval date, placing the earliest possible biosimilar entry at approximately 2035. That is the floor, not a realistic expectation — patent disputes, manufacturing complexity, and the cost of running biosimilar clinical trials routinely push these timelines further out. However, if a manufacturer were to begin biosimilar development now and file with the FDA, the approval process itself typically takes several years. As of early 2026, no company has publicly announced a biosimilar program for lecanemab.
This means that even the 2035 estimate requires a manufacturer to begin working toward that goal within the next few years. Without that pipeline activity, the realistic horizon could extend well past 2035. there is an important caveat worth understanding: patent expiration and biologic exclusivity are not the same thing. Even after the 12-year exclusivity window closes, Eisai and Biogen hold multiple patents covering lecanemab’s composition, manufacturing process, and therapeutic uses. Biosimilar developers would likely need to navigate or challenge those patents, as has happened repeatedly with other biologics. Families hoping for affordable access to lecanemab should not plan their care strategies around the assumption that a lower-cost version is coming soon.
What Formulations of Leqembi Currently Exist?
Leqembi launched in its original form as an intravenous infusion, administered at a clinical infusion center every two weeks. For patients in major metropolitan areas with access to specialized memory care centers, this was feasible. For those in rural areas or with limited mobility, the biweekly IV requirement represented a serious logistical burden — hours of travel, time off work for caregivers, and the physical toll of repeat clinic visits. In August 2025, the FDA approved a subcutaneous injection formulation of lecanemab, marketed as LEQEMBI IQLIK, specifically for maintenance dosing.
This represents a meaningful practical improvement for patients who have already completed the initial IV induction phase. A self-administered or caregiver-administered injection at home removes much of the clinic burden from ongoing treatment. A third formulation — a subcutaneous injection intended for the starting dose phase of treatment — is currently under FDA Priority Review, with a PDUFA action date of May 24, 2026. If approved, this would allow patients to begin and maintain lecanemab therapy without ever needing an IV infusion center, opening the drug to a broader patient population. These formulation advances do not change the cost or availability of biosimilars, but they do improve the day-to-day experience of treatment for those who can access it.

What Does Leqembi Cost and Who Pays for It?
At a list price of approximately $26,500 per year, lecanemab is among the more expensive treatments in the Alzheimer’s space, though it falls within the range seen for other biologics. For comparison, adalimumab (Humira) carries a list price exceeding $80,000 per year before rebates, and some oncology biologics exceed $100,000 annually. In context, lecanemab’s pricing is not unusual for a biologic — but Alzheimer’s care already places enormous financial strain on families, and adding a five-figure annual drug cost creates real hardship. Medicare Part B covers lecanemab for eligible early Alzheimer’s patients enrolled in a qualifying data registry. Standard Medicare beneficiaries face an out-of-pocket cost of approximately $5,300 per year, which reflects the 20% coinsurance typical of Part B after the deductible.
For those with a Medigap supplemental policy that covers coinsurance, this cost could be substantially lower. Medicare Part D does not cover lecanemab because it is administered by infusion, placing it under Part B rather than the prescription drug benefit. The practical tradeoff here is worth stating plainly. Medicare coverage makes lecanemab accessible to a much larger population than would otherwise qualify, but the $5,300 annual cost remains out of reach for many retirees on fixed incomes. Patients without Medicare — those who are younger or covered by private insurance — face a more complicated path that varies by insurer and plan. Eisai offers a patient assistance program, but the scope and eligibility criteria of such programs can change, and families should verify current terms directly with the manufacturer.
What Are the Eligibility and Safety Considerations?
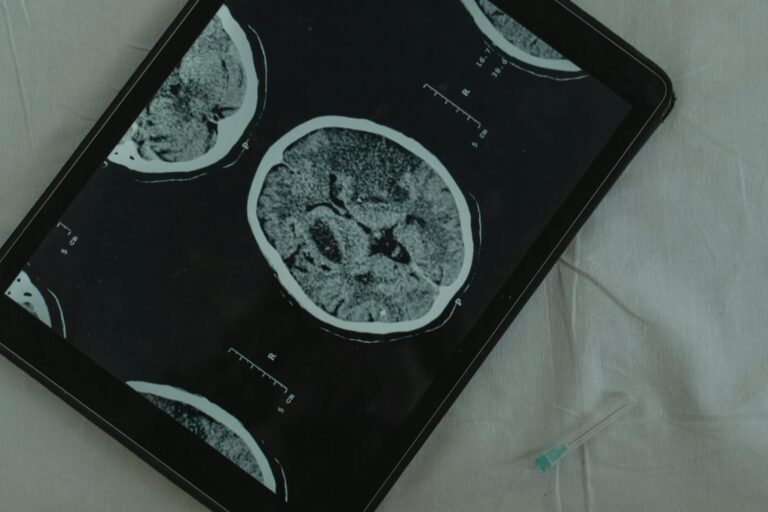
Lecanemab is not appropriate for all Alzheimer’s patients. It is indicated for adults with early-stage Alzheimer’s disease — specifically those with mild cognitive impairment or mild dementia who have confirmed amyloid pathology. Confirming amyloid requires either a PET scan or a cerebrospinal fluid analysis, both of which carry their own costs and logistics. Patients with moderate or advanced Alzheimer’s are not candidates for this treatment. A significant safety concern is amyloid-related imaging abnormalities, known as ARIA — brain swelling or microbleeds that can occur as a side effect of amyloid-targeting therapies.
In clinical trials, ARIA occurred in a meaningful proportion of lecanemab-treated patients. Most cases were asymptomatic and detected only on MRI monitoring scans, but some patients experienced serious symptoms requiring hospitalization. Patients on blood thinners or carrying two copies of the APOE4 gene variant face elevated risk of severe ARIA and require careful risk-benefit discussion with their neurologist. The warning here is direct: the existence of a covered, approved drug does not mean it is right for every patient or every family situation. The clinical benefit demonstrated in trials — a slowing of cognitive decline rather than a reversal — is meaningful but modest. Families should enter conversations with their physician not with the assumption that lecanemab is the obvious choice, but with a clear-eyed understanding of what the drug does, what it risks, and whether the treatment burden is sustainable for their specific circumstances.

Are There Any Lower-Cost Alternatives for Dementia Treatment?
No currently approved drug replicates lecanemab’s mechanism of action at a lower cost. The other approved disease-modifying therapy in this class, donanemab (Kisunla), is also a biologic with no biosimilar, carrying similar pricing. Older Alzheimer’s medications such as donepezil, rivastigmine, memantine, and galantamine are all available as inexpensive generics — donepezil, for example, can be obtained for a few dollars per month — but these drugs work on symptoms and do not slow the underlying disease process the way lecanemab is intended to.
For families who cannot access lecanemab or for whom cost remains prohibitive, the realistic options are these established symptomatic treatments, lifestyle interventions with documented cognitive health benefits, and enrollment in clinical trials investigating next-generation Alzheimer’s therapies. Clinical trial participation can provide access to experimental drugs at no cost while also contributing to the evidence base that will shape future treatment. ClinicalTrials.gov maintains a searchable database of active Alzheimer’s trials by location.
What Should Families Expect in the Coming Years?
The lecanemab landscape will evolve, but not quickly. The subcutaneous formulation currently under FDA review may be approved by mid-2026, making treatment more convenient. Competition within the amyloid-targeting class — primarily from donanemab — may create some market pressure on pricing over time, though neither drug will face biosimilar competition for the foreseeable future.
Medicare coverage policy, which has already shifted toward broader access, could continue to expand or face political revision depending on the regulatory environment. The honest long-term view is that families dealing with early Alzheimer’s today should not wait for a generic or biosimilar version of lecanemab. That option does not exist and will not exist within any clinically relevant timeframe for patients diagnosed now. The actionable steps are navigating current coverage options, understanding eligibility, speaking with a neurologist familiar with the clinical evidence, and making decisions based on what is actually available — not what might eventually be accessible years from now.
Conclusion
As of early 2026, there is no generic or biosimilar version of lecanemab available, and there will not be one for at least a decade under current law. Leqembi remains a brand-name biologic sold exclusively by Eisai and Biogen, protected by 12 years of regulatory exclusivity that runs until approximately 2035. No manufacturer has publicly begun biosimilar development.
The drug is available in two formulations — IV infusion and subcutaneous injection for maintenance — with a third subcutaneous formulation under FDA review. At $26,500 per year list price, Medicare coverage that brings out-of-pocket costs to roughly $5,300 annually for eligible patients is the most realistic path to access for most families. For caregivers and patients researching their options, the key takeaways are these: verify your eligibility for Medicare Part B coverage, confirm amyloid pathology through appropriate testing, discuss ARIA risk and the realistic scope of benefit with a specialist, and do not delay decisions waiting for a lower-cost version that is not on the horizon. The current formulary is what it is, and navigating it well requires accurate information rather than optimism about future drug pricing.
Frequently Asked Questions
Can my doctor prescribe a generic version of lecanemab?
No. No generic or biosimilar version of lecanemab exists. The only available product is Leqembi, the brand-name drug manufactured by Eisai and Biogen.
Why can’t a generic be made for lecanemab the way generics exist for donepezil?
Donepezil is a small-molecule drug that can be chemically replicated. Lecanemab is a biologic — a complex monoclonal antibody produced through living cell cultures. Biologics require biosimilar approval, not generic approval, and that process is far more complex and time-consuming.
When will a biosimilar lecanemab be available?
Not before approximately 2035 at the earliest, based on the 12-year biologic exclusivity period from the 2023 FDA approval. As of early 2026, no company has announced a biosimilar development program for lecanemab.
Does Medicare cover Leqembi?
Yes, Medicare Part B covers lecanemab for eligible patients with early Alzheimer’s who are enrolled in a qualifying data registry. Standard Medicare beneficiaries pay roughly $5,300 per year in coinsurance; those with Medigap coverage may pay less.
Is the subcutaneous version of lecanemab covered the same way as the IV version?
The maintenance subcutaneous formulation (LEQEMBI IQLIK) was approved in August 2025. Coverage terms for the subcutaneous formulation should be verified with Medicare or your insurer directly, as administrative coding and coverage determinations for new formulations can take time to align with established policy.
Are there any cheaper drugs that work the same way as lecanemab?
No. The only other approved drug in the same class — amyloid-targeting biologics — is donanemab (Kisunla), which carries comparable pricing and has no biosimilar either. Older Alzheimer’s medications like donepezil are available cheaply as generics but address symptoms rather than the underlying disease process.