Yes, a primary care doctor can diagnose dementia — and in many cases, they are the first and sometimes only physician involved in making that determination. General practitioners and family medicine doctors are trained to conduct cognitive assessments, review medical history, order relevant lab work, and apply established diagnostic criteria for conditions like Alzheimer’s disease and vascular dementia. For example, if a 74-year-old patient begins missing appointments, repeating the same questions during visits, or shows a noticeable decline from one annual checkup to the next, a primary care physician can initiate and often complete a full diagnostic workup without an automatic referral to a specialist.
That said, the scope of what a primary care doctor can reliably diagnose depends on the complexity of the case. Straightforward presentations of moderate-to-advanced dementia in older adults are well within their purview. But atypical cases — younger patients, rapid progression, unusual symptoms, or suspected rare dementias like Lewy body or frontotemporal dementia — often benefit from neurologist or geriatric psychiatrist involvement. This article covers what primary care physicians actually do in a dementia evaluation, where their limitations lie, when a specialist referral makes sense, and how to navigate the diagnostic process as a patient or family member.
Table of Contents
- What Can a Primary Care Doctor Actually Diagnose When It Comes to Dementia?
- How Primary Care Physicians Conduct a Dementia Evaluation
- When a Primary Care Doctor Should Refer to a Specialist
- The Practical Steps: What to Expect at a Primary Care Dementia Appointment
- Medications, Management, and What Happens After the Diagnosis
- The Role of Neuropsychological Testing
- How Dementia Diagnosis Is Changing — and What That Means for Primary Care
- Conclusion
- Frequently Asked Questions
What Can a Primary Care Doctor Actually Diagnose When It Comes to Dementia?
Primary care physicians are fully qualified to diagnose the most common forms of dementia, particularly Alzheimer’s disease and vascular dementia, which together account for the vast majority of cases. The diagnostic process does not require specialized imaging equipment or a neurology degree — it requires clinical judgment, validated cognitive tools, and the ability to rule out reversible causes of cognitive decline. A family doctor who has known a patient for years actually has a meaningful advantage here: they have a baseline for comparison that a specialist seeing the patient for the first time does not. The standard tools available to primary care physicians include the Mini-Mental State Examination (MMSE), the Montreal Cognitive assessment (MoCA), and the Mini-Cog. These validated screening instruments take between five and fifteen minutes to administer and can detect meaningful cognitive impairment with reasonable sensitivity.
Paired with a structured clinical interview, collateral history from a family member, and basic blood work to rule out thyroid disorders, vitamin B12 deficiency, and other treatable causes, a primary care physician has most of what is needed to make a confident diagnosis. To illustrate: a 78-year-old woman visits her internist after her daughter reports that her mother has been leaving the stove on, getting lost driving routes she has taken for thirty years, and struggling to recall recent conversations. The physician administers the MoCA, which yields a score of 16 out of 30 — well below the threshold suggesting significant impairment. Lab work comes back normal. With no atypical features and a clinical picture consistent with moderate Alzheimer’s, the primary care doctor documents the diagnosis and begins a conversation about management. No specialist referral is required at that stage.

How Primary Care Physicians Conduct a Dementia Evaluation
The dementia evaluation in a primary care setting typically unfolds across one or two appointments, though some physicians integrate it into annual wellness visits when cognitive concerns arise. The first step is almost always ruling out reversible conditions that can mimic dementia: hypothyroidism, vitamin deficiencies, depression, medication side effects, urinary tract infections in older adults, and sleep disorders can all cause memory and cognitive symptoms that resolve with treatment. Skipping this step is a diagnostic error, not a shortcut. Once reversible causes have been excluded, the physician moves to formal cognitive testing and a thorough neurological exam. They will look for changes in gait, reflexes, and coordination, which can point toward specific dementia subtypes.
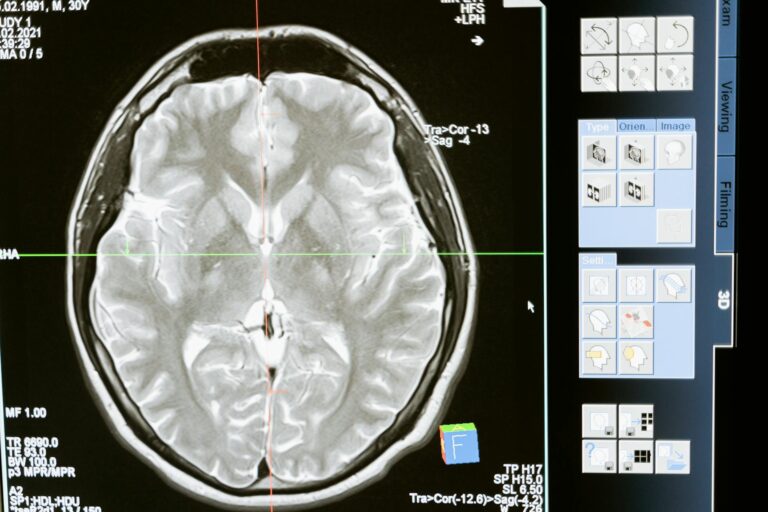
brain imaging — typically a CT scan or MRI — is often ordered to rule out structural causes such as normal pressure hydrocephalus, subdural hematoma, or brain tumors. The MRI also helps differentiate Alzheimer’s-pattern atrophy from the white matter changes seen in vascular dementia. However, there are real limitations in how far a primary care evaluation can go. The MoCA and MMSE are excellent screening tools, but they are not diagnostic in isolation and can produce false positives in people with low education levels or false negatives in highly educated individuals who compensate well. A retired professor with early Alzheimer’s may score in the normal range on standard screening while exhibiting meaningful real-world decline. If the clinical picture and test results do not align, that tension is a signal that a referral may be warranted rather than a diagnosis forced onto an ambiguous case.
When a Primary Care Doctor Should Refer to a Specialist
There are specific clinical scenarios where primary care evaluation reaches its practical limits, and recognizing them is itself a mark of good medical practice. The most important of these is early-onset dementia — cognitive decline presenting before age 65. This population is more likely to have genetic causes, atypical dementia subtypes, or other neurological conditions that require neuropsychological testing and specialist expertise to properly characterize. A 57-year-old engineer who begins making errors at work and showing personality changes deserves more than a brief office screen; a neurologist or geriatric psychiatrist should be involved early. Rapid cognitive decline — significant worsening over weeks rather than years — also warrants urgent specialist referral, in part because it can indicate Creutzfeldt-Jakob disease, autoimmune encephalitis, or paraneoplastic syndromes, which are medical emergencies masquerading as dementia.
Similarly, Lewy body dementia, which presents with fluctuating cognition, visual hallucinations, and Parkinsonian motor features, is frequently misdiagnosed in primary care settings because it does not fit the typical Alzheimer’s pattern. Mistaking it for Alzheimer’s is not just an academic error — certain antipsychotic medications that might be prescribed for behavioral symptoms are dangerous and potentially fatal in Lewy body dementia patients. Behavioral variant frontotemporal dementia (bvFTD) is another condition that primary care physicians often struggle to identify. It presents primarily with personality changes, disinhibition, and loss of empathy rather than memory loss, which means patients are sometimes referred to psychiatrists for depression or personality disorders before anyone thinks to evaluate for dementia. A 62-year-old man who begins making inappropriate comments at family gatherings, stops showering, and starts compulsively eating sweets — while scoring adequately on memory tests — may have bvFTD, not a psychiatric condition. This is the kind of case where neurological referral changes the entire trajectory of care.

The Practical Steps: What to Expect at a Primary Care Dementia Appointment
If you are bringing a parent or spouse to a primary care doctor with cognitive concerns, knowing what to expect helps you make the most of the visit. Before the appointment, document specific examples of concerning behaviors with dates and context — not just “seems forgetful,” but “forgot that her sister died three months ago when we mentioned her yesterday” or “got lost driving to church he has attended for forty years.” Concrete, dated examples carry more diagnostic weight than general impressions and help the physician distinguish normal aging from pathological change. The physician will likely want to speak with the patient alone for part of the visit and with the family separately for another portion. Be prepared for the patient to minimize symptoms or become defensive — this is extremely common and does not mean the concerns are invalid. The collateral history from family members is often more diagnostically useful than the patient’s self-report, particularly in moderate-stage disease where insight is compromised.
Some physicians use structured caregiver questionnaires like the AD8 Dementia Screening Interview, which family members complete before or during the visit. Compared to going directly to a neurologist, starting with a primary care physician has both advantages and tradeoffs. The wait time to see a neurologist can stretch to three to six months in many parts of the United States, while a primary care appointment may be available within days or weeks. For patients with a clear clinical picture, the primary care pathway gets to a diagnosis and treatment planning faster. On the other hand, neurologists have deeper familiarity with the diagnostic nuances, access to more sophisticated testing, and more experience with complex or atypical presentations. The two pathways are not mutually exclusive — primary care can initiate and even complete the diagnosis while also facilitating a neurology referral for ongoing co-management.
Medications, Management, and What Happens After the Diagnosis
Once a dementia diagnosis is made in primary care, the physician’s role expands significantly. Cholinesterase inhibitors such as donepezil (Aricept) and rivastigmine (Exelon), along with memantine for moderate-to-severe Alzheimer’s, are typically initiated and managed by primary care physicians. These medications do not stop or reverse the disease, but they can modestly slow functional decline and improve quality of life in some patients. The decision to start them involves weighing potential side effects — nausea, bradycardia, insomnia — against expected benefit, and requires ongoing monitoring. Behavioral and psychological symptoms of dementia (BPSD) — including agitation, sleep disturbances, depression, and psychosis — represent one of the more challenging aspects of primary care dementia management. Non-pharmacological approaches should always be tried first: structured routines, reduced environmental stimulation, caregiver training, and music therapy have meaningful evidence behind them.
When medications are necessary, the selection requires caution. Low-dose SSRIs for depression and agitation, melatonin for sleep, and careful use of antipsychotics all carry significant risks in older adults, and primary care physicians vary considerably in their comfort managing these symptoms. An important warning here: the black-box warning on antipsychotics for elderly patients with dementia is not theoretical. These medications carry an increased risk of stroke and death in this population. If a primary care physician prescribes an antipsychotic for a dementia patient’s behavioral symptoms without documenting that non-pharmacological approaches were tried first and without discussing the risks with the family, that is worth questioning. Patients and families should feel empowered to ask about alternatives before agreeing to these medications.

The Role of Neuropsychological Testing
In cases where the clinical picture is unclear — normal cognitive screening scores despite real-world decline, highly educated patients who may be masking impairment, or cases where the differential includes mild cognitive impairment versus early dementia — neuropsychological testing provides a level of detail that no brief office screen can match. A full neuropsychological battery takes several hours and evaluates memory, attention, executive function, language, and visuospatial abilities with standardized, age-normed instruments.
Primary care physicians can order a neuropsychological referral without going through a neurologist, though in practice many do not. A 68-year-old retired attorney who reports memory concerns but scores 27/30 on the MoCA might seem fine on paper, but neuropsychological testing might reveal significant deficits in delayed recall and processing speed that fall two standard deviations below age-matched peers — a finding consistent with early Alzheimer’s that the brief screen missed. For families in this situation, asking specifically for a neuropsychology referral rather than waiting to see whether symptoms worsen is a reasonable and underused option.
How Dementia Diagnosis Is Changing — and What That Means for Primary Care
The landscape of dementia diagnosis is shifting in ways that will increasingly affect what happens at the primary care level. Blood-based biomarkers for Alzheimer’s — particularly plasma phosphorylated tau 217 (p-tau217) — are now available through commercial labs and can identify amyloid pathology with high accuracy before significant symptoms appear. These tests do not replace clinical judgment, but they may soon become a routine part of primary care evaluation in the same way that PSA testing became standard for prostate cancer screening, with all the associated debates about overdiagnosis and downstream consequences.
New disease-modifying therapies like lecanemab and donanemab, while currently administered through specialist centers, are creating pressure on the entire diagnostic pathway because they require confirmation of amyloid pathology via PET scan or cerebrospinal fluid analysis before treatment can begin. This means that a dementia diagnosis from a primary care doctor, while valid and important, may need to be augmented with specialist-level biomarker testing for patients who want to access emerging treatments. The role of primary care in dementia is not diminishing — if anything, it is becoming more central — but the complexity of what that role requires is growing alongside the science.
Conclusion
A primary care doctor can and routinely does diagnose dementia, particularly in its most common forms. The evaluation they conduct — ruling out reversible causes, applying validated cognitive screens, ordering appropriate imaging, and gathering collateral history — is thorough enough to support a confident diagnosis in the majority of cases. Patients and families do not need to wait months for a specialist appointment to get answers when a knowledgeable and attentive primary care physician can provide them.
Where primary care has limits, those limits are identifiable: atypical presentations, young-onset dementia, rapid decline, suspected Lewy body or frontotemporal dementia, and ambiguous early-stage cases all benefit from specialist input. The most effective path forward usually involves a primary care physician who initiates the evaluation, remains the central coordinator of ongoing care, and refers strategically rather than reflexively. If you are worried about a loved one’s cognitive health, starting with the primary care doctor is not settling for less — it is the right first step.
Frequently Asked Questions
Does a primary care doctor need to refer you to a neurologist to diagnose dementia?
No. In most straightforward cases, a primary care physician can complete the full diagnostic evaluation and make a dementia diagnosis without a neurologist’s involvement. Referrals are appropriate for atypical, complex, or early-onset cases.
What cognitive tests does a primary care doctor use to diagnose dementia?
The most commonly used tools are the Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), and the Mini-Cog. These are brief, validated instruments that can be administered in a standard office visit.
Can a primary care doctor prescribe Alzheimer’s medications?
Yes. Cholinesterase inhibitors like donepezil and rivastigmine, as well as memantine, are all prescribable by primary care physicians and are frequently initiated and managed in that setting.
What if the primary care doctor says everything is normal but the family still sees a problem?
Trust the clinical observations. If a brief office screen appears normal but real-world function is clearly declining, request a formal neuropsychological evaluation. Brief screens can miss early dementia, especially in highly educated individuals.
How long does a primary care dementia evaluation take?
It often spans one or two appointments. The first visit may focus on gathering history and ruling out reversible causes; the second may include formal cognitive testing and a review of lab results and imaging.
Is it helpful to bring a family member to the primary care appointment for dementia concerns?
Very much so. A family member who can describe specific behavioral changes, provide timeline information, and offer a collateral history independent of the patient significantly improves diagnostic accuracy. Many physicians will ask to speak with the family member separately.