Contoured cushions are the best shape for dementia postural stability. Clinical seating specialists consistently recommend contoured designs over flat or basic foam options because they stabilize the pelvis and lower extremities, which in turn keeps the trunk upright and prevents the slumped, twisted postures that lead to falls. A flat, immersion-only cushion might feel comfortable initially, but it lacks the structural support that someone with dementia needs “” particularly when they doze off in their chair and their muscles stop actively working to hold them upright. This matters more than most caregivers realize.
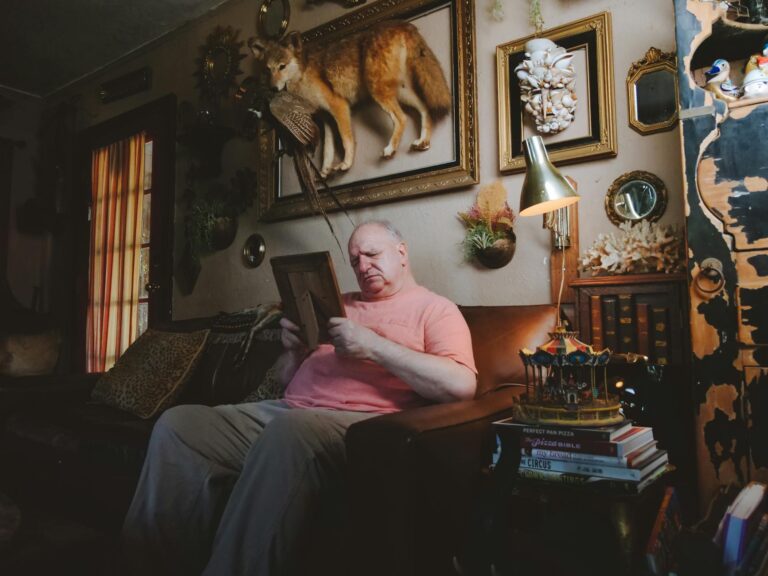
Between 60 and 80 percent of people with dementia fall each year, a rate two to three times higher than cognitively healthy older adults. Dementia itself changes brain shape and density in ways that disrupt the neural pathways responsible for processing sensory information and adjusting posture. A person with advancing dementia gradually loses proprioception “” the internal sense of where their body is in space “” which means they need external support systems to do what their brain no longer can. In one documented clinical case, providing properly immersed and enveloped positioning enabled a client with advanced dementia to resume eating finger foods and regain use of his arms, a quality-of-life improvement that started with the right cushion. This article breaks down the specific cushion shapes available, explains how wedge and pommel designs address different postural problems, covers the cocoon approach to sensory feedback, and offers practical guidance on density, firmness, and when to call in a professional assessment.
Table of Contents
- Why Does Cushion Shape Matter So Much for Dementia Postural Stability?
- Contoured vs. Flat Cushions “” What the Evidence Actually Shows
- Wedge and Pommel Shapes “” Solving Specific Postural Problems
- The Cocoon Approach “” How Envelopment Provides Sensory Stability
- Getting the Density and Firmness Right “” A Common Mistake
- Lateral Supports and the Problem of Sideways Leaning
- When to Seek Professional Assessment
- Conclusion
- Frequently Asked Questions
Why Does Cushion Shape Matter So Much for Dementia Postural Stability?
The connection between cushion shape and postural stability in dementia is more direct than most people expect. Dementia does not just affect memory “” it physically alters the brain in ways that compromise balance and body positioning. In postural stability tests, dementia groups showed 32 percent poorer performance than control groups without cognitive impairment. A 2025 study published in the Journal of the American Medical Directors Association went further, demonstrating that postural sway characteristics during static standing can actually distinguish between types of dementia, including Alzheimer’s disease, Lewy body dementia, and vascular dementia. The postural system is that deeply affected. This is where cushion shape becomes a clinical decision rather than a comfort preference. The NHS advises that incorrect seating significantly affects health “” poor posture such as slouching and sliding constricts the chest cavity and abdomen, which can impair breathing and digestion.
For someone with dementia who cannot consciously correct their own posture, the cushion has to do that corrective work. A contoured cushion creates defined channels for the pelvis and thighs, holding the body in alignment passively. A flat cushion, by contrast, provides a uniform surface that offers no positional guidance. The difference is roughly analogous to sleeping on a shaped orthopedic pillow versus a folded towel “” one holds your neck where it should be, the other leaves it to chance. The comparison matters because many standard-issue care home chairs still come with basic flat foam cushions. These are adequate for cognitively healthy residents who can shift their weight and reposition themselves. They are not adequate for someone whose brain has lost the ability to register that they are sliding sideways or slumping forward.

Contoured vs. Flat Cushions “” What the Evidence Actually Shows
Contoured cushions are explicitly recommended by clinical seating experts for dementia care, while immersion-only flat cushions are explicitly not recommended. The reasoning from Spex Seating’s dementia clinical guidance is straightforward: flat cushions do not provide a stable base of support, and when a resident falls asleep with muscles no longer activated, maximum stability becomes critical. A contoured cushion maintains pelvic alignment whether the person is awake and engaged or dozing after lunch. However, contouring alone is not enough if the contour does not match the individual. A cushion contoured for a larger frame will not stabilize a smaller person “” they will rattle around inside the channels rather than being held by them. This is where products like the ROHO Contour Select Cushion become relevant.
It uses multiple cell heights with ISOFLO Memory Control to provide postural control and can correct or accommodate postural asymmetries of up to one inch. The Spex Classic SuperHigh Contour Cushion takes a modular approach, allowing clinicians to adjust the contour configuration. Both represent the principle that contouring must be fitted, not generic. There is a caveat worth noting. Contoured cushions can make transfers more difficult. The raised edges and channels that hold someone in proper alignment also create barriers when trying to slide them to the edge of the seat for standing or transferring to a bed. Caregivers need to be trained on proper transfer techniques with contoured seating, and in some cases, a slightly less aggressive contour may be chosen to balance stability with practical caregiving needs.
Wedge and Pommel Shapes “” Solving Specific Postural Problems
Not every postural issue calls for the same solution. Two of the most common problems in dementia seating “” forward sliding and leg misalignment “” each have a targeted cushion shape designed to address them. Wedge-shaped cushions are thicker at the front and thinner at the back, creating a gentle slope that tilts the pelvis slightly backward. This directly counteracts the forward thrusting and sliding that many dementia patients exhibit. Forward sliding is not just uncomfortable “” it is dangerous. A person who slides far enough forward can slip out of the chair entirely, and the slouched posture compresses the abdomen and chest.
Pommel cushions address a different problem: they feature a raised ridge between the thighs that abducts and properly aligns the legs. Without this correction, “wind-swept legs” “” where both legs fall to one side “” can cause the hips to rotate, the spine to twist, and the head to drop. What looks like a minor leg positioning issue cascades upward through the entire body. Combined wedge-pommel designs are widely available commercially and address both problems simultaneously. Products like the Protekt Foam Wedge with Pommel Cushion provide the anti-slide angle and the leg separation in a single unit. For someone who both slides forward and has leg alignment issues “” which is common in mid-to-late stage dementia “” this combination avoids the need to stack multiple positioning aids that can shift and bunch up during the day.
The Cocoon Approach “” How Envelopment Provides Sensory Stability
One of the more nuanced developments in dementia seating is the cocoon or envelopment approach. Rather than simply holding someone in place with rigid contours, cocoon-like surfaces conform to the body and create what Seating Matters describes as a “hug” “” providing sensory feedback and stability without creating pressure points. This approach is particularly important for people with dementia because of their reduced proprioception. When the brain can no longer accurately process where the body is in space, a surface that wraps around the body provides constant tactile feedback “” effectively replacing the internal sensory information that has been lost.
Spex Seating’s clinical guidance notes that the combination of immersion and envelopment “” the body sinking into a shaped surface that conforms around it “” provides proprioceptive feedback that helps reduce distress and agitation. This is a meaningful distinction: it is not just about preventing falls, but about reducing the anxiety and restlessness that often accompany poor positioning. The tradeoff with highly enveloping surfaces is heat retention. Materials that conform closely to the body tend to trap warmth and moisture, which can increase the risk of skin breakdown over long sitting periods. Gel-infused foams and breathable covers can mitigate this, but caregivers should monitor skin condition more closely when using high-envelopment cushions, especially during warmer months or in facilities where ambient temperature runs high.
Getting the Density and Firmness Right “” A Common Mistake
Cushion firmness is where many well-intentioned caregivers go wrong. The instinct is to choose the softest cushion available, reasoning that comfort equals quality of care. But cushion density must be carefully balanced: too soft and the individual sinks in and cannot reposition themselves; too hard and they develop pressure sores. Both extremes create problems that are worse than the issue they were trying to solve. A person with dementia who sinks deeply into an overly soft cushion loses whatever residual postural control they still have.
They cannot push themselves upright because there is nothing firm to push against. They also cannot shift their weight to relieve pressure, which paradoxically means that the “comfortable” soft cushion can cause more skin damage than a firmer alternative. On the other end, a cushion that is too firm provides no pressure distribution at all, concentrating the body’s weight on the bony prominences of the pelvis “” the ischial tuberosities “” where pressure injuries most commonly develop. The practical warning here is that cushion density needs change over time as dementia progresses. A cushion that was appropriately firm when someone still had moderate trunk control may become too firm when they lose muscle tone and spend more time in a static seated position. Regular reassessment is essential, and this is one reason why occupational therapists perform evaluations checking posture, muscle tone, and flexibility before prescribing therapeutic cushions, back supports, or tilt-in-space wheelchairs tailored to the individual’s current needs.

Lateral Supports and the Problem of Sideways Leaning
Leaning persistently to one side is among the most common postural issues in dementia care, and it cannot be solved by the seat cushion alone. Lateral supports “” removable side wedges or bolsters that attach to the chair “” improve posture and help individuals feel more supported. Without them, a person who lists to one side will continue doing so regardless of how well-contoured the seat cushion is, because the forces pulling them sideways are acting on the trunk, not the pelvis.
The combination of a contoured seat cushion for pelvic stability and lateral supports for trunk stability addresses the full picture. However, lateral supports should not be so rigid or tightly positioned that they restrict all movement. Some ability to shift weight is necessary for comfort and skin health. The goal is guided support, not immobilization “” a distinction that matters both clinically and ethically in dementia care.
When to Seek Professional Assessment
The information in this article can help caregivers understand what to look for and what to ask about, but cushion selection for someone with dementia should ultimately involve a professional assessment. Occupational therapists and physiotherapists who specialize in seating can evaluate the specific postural challenges an individual faces “” which may include asymmetries, contractures, or tone abnormalities that are not obvious to an untrained eye. As research continues to deepen our understanding of how dementia affects postural control “” including the 2025 findings that postural sway patterns differ across dementia types “” seating interventions are likely to become more condition-specific.
What works for someone with Alzheimer’s-related postural decline may differ from what benefits someone with Lewy body dementia. For now, the foundational principle remains: contoured, properly fitted cushion support is not a luxury in dementia care. It is a clinical necessity that affects breathing, digestion, skin integrity, and day-to-day quality of life.
Conclusion
The evidence points clearly toward contoured cushions as the best shape for dementia postural stability, with wedge and pommel features addressing specific problems like forward sliding and leg misalignment. The cocoon approach adds another dimension by providing the sensory feedback that compensates for lost proprioception. Flat, immersion-only cushions do not provide adequate stability for this population, particularly during periods of sleep or reduced muscle activation.
Choosing the right cushion is not a one-time decision. As dementia progresses and postural needs change, the cushion should be reassessed and adjusted. Work with an occupational therapist who understands seating for cognitive impairment, pay attention to how the person sits throughout the entire day rather than just during initial fitting, and remember that the right cushion does more than prevent falls “” it can restore function, reduce agitation, and meaningfully improve quality of life.
Frequently Asked Questions
Can a regular memory foam cushion work for someone with dementia?
Standard memory foam provides immersion but not contouring or structural support. It allows the body to sink in without guiding the pelvis or thighs into proper alignment. For someone with dementia-related postural instability, a shaped or contoured cushion is a significantly better choice than flat memory foam.
How often should a dementia seating cushion be replaced?
Most therapeutic cushions maintain their supportive properties for 18 to 24 months with daily use, though this varies by material. More importantly, the person’s needs should be reassessed every 6 to 12 months as dementia progresses, because a cushion that fit correctly a year ago may no longer match their current postural profile.
Is a wedge cushion enough on its own for dementia postural support?
A wedge addresses forward sliding specifically but does not provide lateral stability or full pelvic contouring. For someone with multiple postural issues “” which is common in moderate to advanced dementia “” a wedge alone is usually insufficient. Combined wedge-pommel designs or fully contoured systems offer more comprehensive support.
Do contoured cushions work in any chair?
Contoured cushions work best in chairs with appropriate seat depth and width. Placing a contoured cushion in an oversized chair reduces its effectiveness because the cushion cannot stabilize the pelvis if the person has room to shift around it. Chair and cushion should be assessed together as a system.
What is the difference between a contoured cushion and a tilt-in-space wheelchair for dementia?
They serve complementary functions. A contoured cushion stabilizes the pelvis and thighs at the seating surface. A tilt-in-space wheelchair changes the angle of the entire seat relative to gravity, redistributing weight and reducing the forces that cause forward sliding. For advanced postural needs, both may be prescribed together.