The best cushion design for reducing confusion in dementia patients combines three elements: solid high-contrast colors in the warm spectrum, tactile sensory features that keep hands occupied, and enough structural support to provide proprioceptive feedback so the person feels physically grounded. This is not guesswork. A meta-analysis of three randomized controlled trials involving 135 dementia patients found that sensory interventions were the only type of non-pharmacological intervention to achieve a statistically significant reduction in agitation, with a standardized mean difference of -1.07 (95% CI -1.76 to -0.38), published in Aging and Mental Health in 2009. A cushion that gets the color wrong, lacks texture, or fails to support posture is not just uncomfortable — it can actively make confusion and distress worse. Consider a common scenario in a care home: a resident with moderate Alzheimer’s is seated in a patterned armchair that blends into a similarly patterned carpet.
The cushion is flat, featureless, and offers no sensory engagement. The resident becomes agitated, tries to stand, and falls. Replacing that setup with a solid-colored, high-contrast cushion featuring tactile elements like ribbons and varied fabric textures, paired with lateral supports to correct posture, addresses multiple drivers of confusion simultaneously. It gives the brain clear visual information, something meaningful to do with the hands, and physical feedback about where the body is in space. This article breaks down the specific design features that research supports — from color selection and sensory stimulation to pressure management and familiar aesthetics — and flags where the evidence is strong, where it is limited, and where caregivers need to make practical tradeoffs.
Table of Contents
- Why Does Cushion Design Affect Confusion in Dementia Patients?
- How Color and Contrast in Cushion Fabrics Reduce Visual Confusion
- The Role of Tactile and Sensory Cushion Features
- Choosing Between Sensory, Postural, and Pressure-Relief Cushion Designs
- Pressure Ulcer Risks That Make Cushion Selection a Medical Decision
- Why Familiar, Domestic-Style Cushions Outperform Clinical Designs
- Research Gaps and the Future of Cushion Design for Dementia Care
- Conclusion
Why Does Cushion Design Affect Confusion in Dementia Patients?
Dementia does not just erode memory. It degrades the sensory systems that help a person understand where they are and what is happening around them. Many people with dementia have reduced proprioception and bodily sensation, meaning they may not feel the chair beneath them in the way a cognitively healthy person does. When the brain cannot reliably process where the body is in space, the result is often distress, restlessness, and escalating agitation. Cushions that provide what clinicians call “envelopment and immersion” deliver proprioceptive feedback that reduces this confusion by giving the body clear, consistent sensory signals.
The connection between cushion design and behavior is also economic. Research published in a Health Technology Assessment found that sensory interventions are relatively cost-effective: the incremental cost per unit reduction on the Cohen-Mansfield Agitation Inventory ranged from just £24 to £143, compared to £162 to £3,480 for activity-based interventions. For care facilities operating on tight budgets, this means a well-designed sensory cushion can deliver measurable behavioral improvements at a fraction of the cost of structured activity programs. The comparison is striking — a tactile cushion costing under £50 can outperform a staffed intervention costing thousands per patient. However, this does not mean any cushion with a few buttons sewn on will do the job. The design details matter enormously, and a cushion that gets the sensory balance wrong — too much stimulation, the wrong colors, inadequate support — can increase confusion rather than reduce it.

How Color and Contrast in Cushion Fabrics Reduce Visual Confusion
alzheimer‘s disease specifically impairs color discrimination, particularly in the blue-green range, while perception of reds and yellows remains relatively preserved. Contrast sensitivity is also diminished, meaning that color differences must be significantly stronger for a person with dementia to perceive them. This has direct implications for cushion design: a pale blue cushion on a grey chair may be functionally invisible to someone with moderate Alzheimer’s, creating a visual environment where the person cannot distinguish where to sit or what is supporting them. Research from the Dementia Alliance International and design studies consistently recommend solid, high-contrast colors on cushions and seating. Patterned fabrics should be avoided outright — they can be disorienting and stress-inducing for people with dementia, as the brain attempts and fails to make sense of complex visual information. Chair upholstery should contrast with the floor so patients can distinguish furniture from their surroundings.
A warm red or deep amber cushion on a light-colored chair, placed against a contrasting floor, gives the brain the clearest possible information about where the seat is and where the person’s body ends and the environment begins. There is a nuance here, though. While strong contrast is critical, the colors themselves should not be harsh or overstimulating. Studies on healthcare facility design indicate that soft pastel tones — light blues, greens, and lavenders — create calming environments that reduce anxiety and agitation. The practical solution is to use warm, solid colors for the cushion itself to ensure visibility, while keeping the broader room palette soft and muted. If a facility paints walls in aggressive primary colors thinking “high contrast equals good,” they risk creating an overstimulating environment that trades one source of confusion for another.
The Role of Tactile and Sensory Cushion Features
Tactile or fidget cushions use ribbons, buttons, zippers, different fabric textures, and embroidery to provide soothing hand occupation and stimulation. The principle is straightforward: when a person with dementia has something purposeful and calming to do with their hands, they are less likely to escalate from mild unease into agitated or aggressive behavior. Research published through Taylor and Francis on sensory design for dementia care indicates that these features help reduce the escalation of negative emotions, intercepting the behavioral spiral before it reaches a crisis point. A practical example: a care home in the UK introduced cushions with a patchwork of corduroy, satin, fleece, and cotton panels, with sewn-on buttons and short ribbon loops along the edges. Staff reported that residents who had previously picked at their clothing or the arms of chairs — a common sign of under-stimulation — redirected that energy to the cushion. The picking behavior decreased, and with it the skin damage and distress that accompanied it.
The cushion did not cure anything, but it gave the hands something safe and engaging to do. The key limitation here is individual variation. A person with advanced dementia and severe tactile defensiveness may find certain textures distressing rather than soothing. Buttons or small attachments can also pose a choking risk for patients who mouth objects. Any sensory cushion needs to be assessed for the specific individual using it, and features like buttons should be securely fastened and regularly inspected. A sensory cushion designed for one person’s comfort profile may be entirely wrong for another’s.

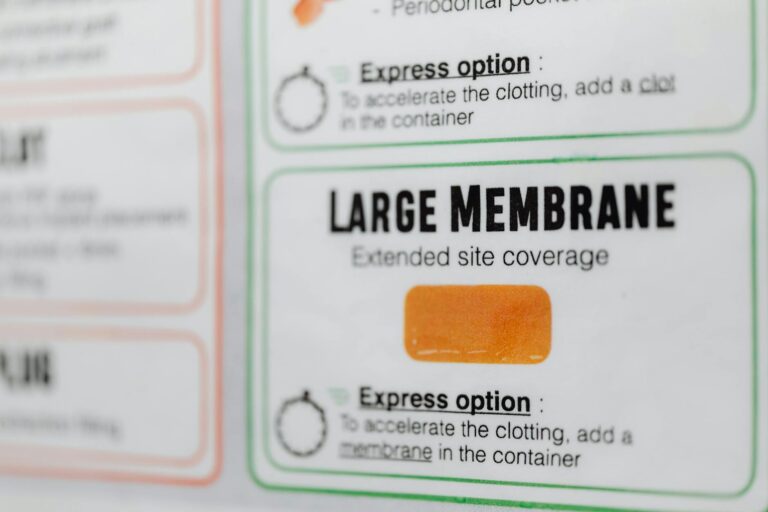
Choosing Between Sensory, Postural, and Pressure-Relief Cushion Designs
In practice, caregivers face a tradeoff between three types of cushion function: sensory engagement, postural support, and pressure relief. Few single cushions do all three well, and understanding what a particular patient needs most should drive the choice. For a person whose primary issue is agitation and restlessness, a sensory cushion with varied textures and fidget elements is the priority. For someone who consistently slumps to one side — common in patients who lack the cognitive capacity to recognize when they are listing — removable lateral supports and wedge cushions that correct posture are more urgent. These patients need proprioceptive grounding more than hand stimulation. And for patients who sit for extended periods and are at high risk for pressure injuries, cool-gel or alternating air-system cushions become medically necessary.
Dementia patients face roughly double the risk of developing pressure ulcers compared to those without dementia, with an adjusted relative risk of 2.01 for Alzheimer’s patients specifically. This is not a comfort issue — it is a survival issue. Median survival for patients with both pressure ulcers and dementia was just 63 days, compared to 117 days for pressure ulcer patients without dementia. The ideal approach layers these functions. A tilt-and-recline seating system with a pressure-redistributing cushion base, topped with a removable sensory cover that can be washed and replaced, addresses all three needs. However, cost and practicality intervene. In many home care settings, the best realistic option is a high-quality pressure-relief cushion combined with a separate lap-sized sensory mat, allowing the caregiver to address both needs without compromising either.
Pressure Ulcer Risks That Make Cushion Selection a Medical Decision
The stakes of getting cushion design wrong extend well beyond comfort or behavioral management. Pressure ulcer prevalence in nursing homes sits at a pooled estimate of 11.6% across 30 studies involving 355,784 patients. Global decubitus ulcer cases rose from 300,442 in 1990 to 645,588 in 2021, with the majority occurring in people aged 60 and older. For dementia patients specifically, the risk is compounded by immobility, inability to communicate pain, and reduced awareness of the need to shift position. The 63-day median survival figure for patients with co-occurring pressure ulcers and dementia should be a wake-up call for anyone selecting seating.
A cushion that looks nice and has pleasant textures but does not adequately redistribute pressure is potentially dangerous for a patient who sits in the same chair for eight or more hours a day. Cool-gel cushions and alternating air systems work by preventing sustained pressure on any single area of tissue, and they are recommended specifically for dementia patients with extended sitting times. A warning: pressure-relief cushions that use alternating air cells can sometimes produce subtle movement or noise that unsettles some dementia patients. The sensation of the surface shifting beneath them may trigger anxiety in individuals who are already disoriented. Caregivers should monitor the patient’s response when introducing any new pressure-relief system, and be prepared to switch to a static gel or foam alternative if the dynamic surface causes distress. The medical benefit of pressure prevention must be balanced against the behavioral cost of increased confusion.

Why Familiar, Domestic-Style Cushions Outperform Clinical Designs
Cushion and furniture design that mirrors familiar domestic settings has a documented calming effect and reduces confusion and disorientation. Research on dementia-friendly design identifies three overarching principles for environments: manageable cognitive load, clear sequencing, and an appropriate level of stimulation.
A cushion that looks like it belongs in a hospital — vinyl-covered, institutional in color, stripped of personality — violates all three by signaling an unfamiliar environment and providing no comforting associations. A practical application: rather than purchasing clinical-looking sensory cushions, some care providers have found success using cushion covers made from fabrics that resemble home furnishings — a floral cotton that might have been found in the person’s own living room decades ago, or a tartan wool reminiscent of a family blanket. The sensory and postural elements are built into the cushion’s structure, but the outward appearance says “home” rather than “facility.” This approach works because it reduces the cognitive load of interpreting the environment, allowing the person to feel settled rather than displaced.
Research Gaps and the Future of Cushion Design for Dementia Care
The honest assessment is that the evidence base for cushion-specific design in dementia remains limited. Most published research focuses on broader environmental and seating design rather than cushions in isolation, and the studies that do exist tend to be small, with significant heterogeneity in methods and populations. The 2009 meta-analysis that demonstrated sensory intervention effectiveness, while compelling, included only 135 participants across three trials and showed substantial heterogeneity (I²=68%).
Further methodologically rigorous trials are needed, particularly on optimal therapy duration and long-term effects of sensory cushion use. What is emerging, however, is a more integrated approach to dementia seating that treats the cushion not as an isolated object but as part of a system — combining pressure management, sensory engagement, postural support, visual design, and familiar aesthetics into a coherent whole. As the population ages and dementia prevalence grows, the demand for evidence-based cushion design will intensify. The research that exists today strongly suggests that thoughtful cushion design can reduce agitation cost-effectively, but the field needs larger trials, standardized outcome measures, and head-to-head comparisons of specific design features to move from “promising” to “proven.”.
Conclusion
The best cushion design for reducing confusion in dementia patients is not a single product but a combination of evidence-supported features: solid warm-spectrum colors with high contrast against surrounding furniture, tactile elements that provide safe hand occupation, structural support that delivers proprioceptive feedback, pressure-redistribution technology for patients with extended sitting times, and an outward appearance that feels familiar and domestic rather than clinical. The research consistently shows that sensory interventions reduce agitation more effectively and more affordably than most other non-pharmacological approaches, and that getting visual and postural design wrong can actively worsen confusion. For caregivers making decisions now, the practical steps are clear: assess the individual patient’s primary needs — behavioral, postural, or medical — and prioritize accordingly. Avoid patterned fabrics.
Choose warm, solid colors. Ensure the cushion contrasts with its surroundings. Add tactile features appropriate to the person’s cognitive stage and risk profile. And take pressure ulcer prevention seriously, because for dementia patients, it is not just about comfort — it is about survival. Where the evidence is thin, err on the side of simplicity, familiarity, and close observation of how the individual responds.