The first changes in the brain before dementia symptoms appear are not what most people expect — they are not memory lapses or confusion, but silent molecular events that begin up to 20 years before any cognitive problems surface. Amyloid-beta proteins start clumping together, the brain’s waste-clearing channels become sluggish, inhibitory neurons begin dying off, and the very shape of the brain starts shifting in subtle but measurable ways. In people carrying Alzheimer’s-linked genes, researchers have found amyloid plaques forming as early as their late 20s, a full 15 years before any cognitive symptoms emerged. These discoveries have fundamentally changed how scientists think about dementia — not as a disease that strikes suddenly in old age, but as a slow-building process rooted in midlife biology.
What makes this research so urgent is that the window for intervention may be far wider than anyone previously assumed. A landmark NIH study published in *Nature Neuroscience* in October 2024 revealed that Alzheimer’s damages the brain in two distinct phases — a long, quiet preclinical phase and a rapid, destructive symptomatic phase. If the silent phase can be detected and disrupted, the second phase might be delayed or even prevented. This article breaks down exactly what those earliest brain changes look like, which ones are now detectable with existing technology, and what recent research suggests about protecting yourself during the years when damage is accumulating but symptoms have not yet appeared.
Table of Contents
- What Are the Earliest Detectable Brain Changes Before Dementia Symptoms Appear?
- How Brain Structure and Shape Shift Years Before Cognitive Decline
- Clogged Brain Drains — A Newly Discovered Early Warning Sign
- Personality Changes Before Memory Loss — What to Actually Watch For
- Disrupted Brain Connectivity — The Invisible Breakdown
- What the Two-Phase Model Means for Early Detection
- Cognitive Training and the Future of Dementia Prevention
- Conclusion
- Frequently Asked Questions
What Are the Earliest Detectable Brain Changes Before Dementia Symptoms Appear?
The earliest measurable change in the Alzheimer’s disease process is the accumulation of amyloid-beta protein. According to researchers at USC’s Alzheimer’s Therapeutic Research Institute, elevated amyloid-beta levels appear in blood and spinal fluid years before any symptoms manifest, and gray matter loss in Alzheimer’s-affected brain regions is also detectable at this stage. For a long time, scientists believed these protein deposits were the sole early event. But the NIH study analyzing 84 brains through the Seattle Alzheimer’s Disease Brain Cell Atlas showed a more complex picture. During the silent preclinical phase, several things happen simultaneously: amyloid plaques accumulate slowly, the brain’s immune system activates, myelin — the insulation around nerve fibers — sustains damage, and a specific type of neuron begins to die. That last finding was a genuine surprise.
Researchers had long assumed that excitatory neurons were the first casualties of Alzheimer’s. Instead, the NIH study found that somatostatin inhibitory neurons — the cells responsible for regulating and calming neural activity — are the first to go. This matters because inhibitory neurons act like brakes on the brain’s signaling system. When they fail, neural circuits can become overactive and chaotic, potentially accelerating further damage. Think of it as losing the referees in a game — the players keep going, but the coordination falls apart. This reframing has significant implications for drug development, because targeting amyloid alone may miss half the problem if myelin damage and inhibitory neuron loss are happening in parallel.

How Brain Structure and Shape Shift Years Before Cognitive Decline
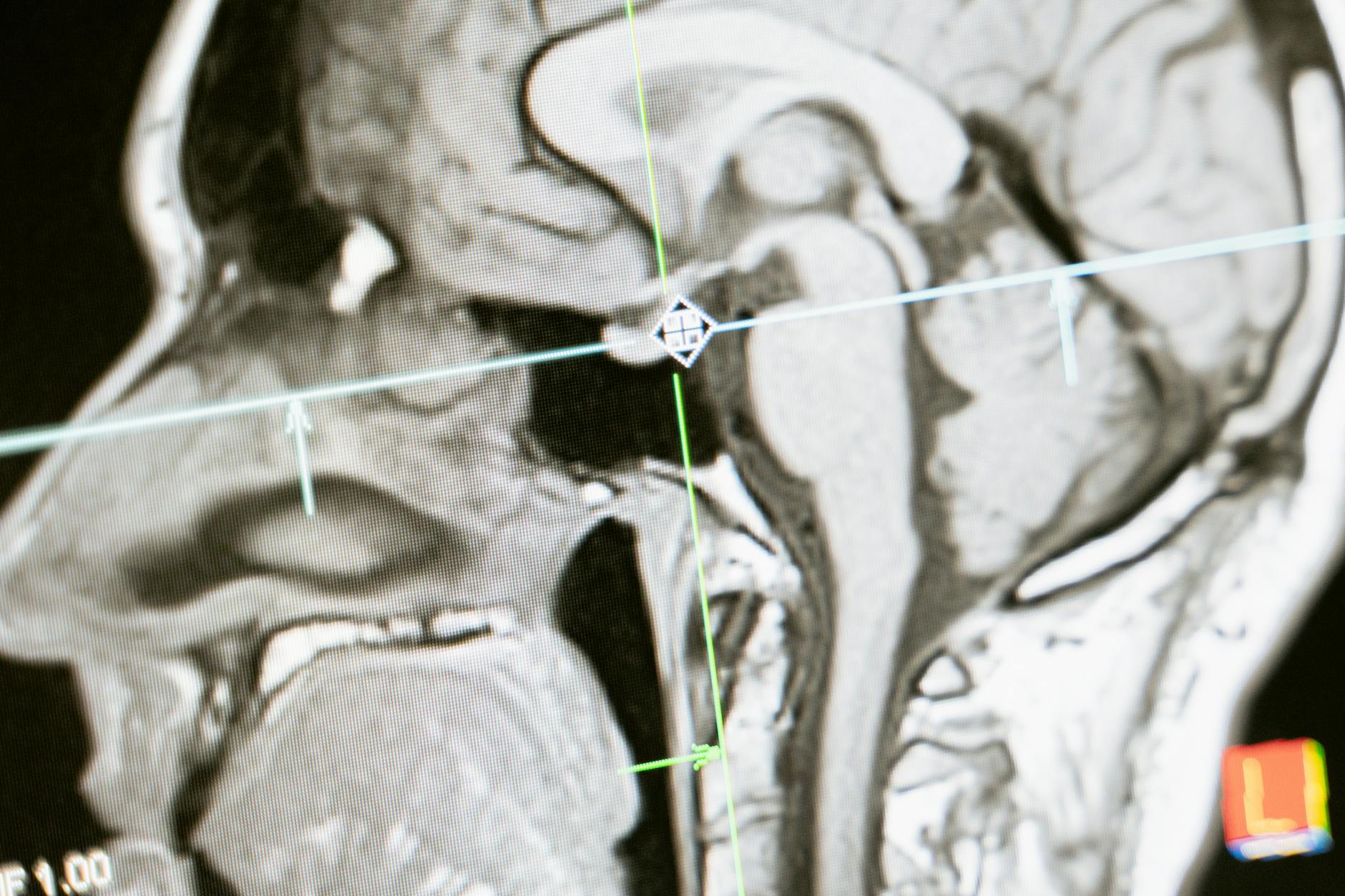
Beyond molecular changes, the physical architecture of the brain begins to warp during the preclinical period. A UC Irvine study from October 2025 found that aging causes a characteristic pattern of brain deformation: inferior and anterior regions expand outward, while superior and posterior regions contract inward. These geometric shifts are not merely cosmetic — they correlate directly with cognitive decline and increase the vulnerability of the entorhinal cortex, one of the very first brain regions damaged in Alzheimer’s disease. The entorhinal cortex is critical for memory formation and spatial navigation, which is why getting lost in familiar places is sometimes an early behavioral sign. A separate study from July 2025 demonstrated that a single midlife MRI can identify rapid brain aging that signals disease long before symptoms emerge.
However, there is a limitation worth noting: not everyone whose brain shows accelerated aging will develop dementia, and not everyone with a normal-looking scan is in the clear. Brain shape changes reflect statistical risk, not individual certainty. A person with significant brain volume loss at age 55 might never develop Alzheimer’s if other protective factors — cardiovascular health, cognitive reserve, genetics — are working in their favor. Conversely, someone with a relatively normal scan could still be accumulating amyloid and tau in ways that structural imaging does not capture. This is why researchers emphasize that no single biomarker is sufficient on its own. The combination of structural, molecular, and functional measures provides a far more reliable picture than any one test.
Clogged Brain Drains — A Newly Discovered Early Warning Sign
One of the most striking recent findings involves the brain‘s waste-clearing infrastructure. A 2025 study from NTU Singapore, published in *Neurology* on August 22, 2025, found that enlarged perivascular spaces — essentially clogged drainage channels around blood vessels — are significantly more common in people with mild cognitive impairment. These channels are part of the glymphatic system, which flushes toxic waste products like amyloid and tau out of the brain, primarily during deep sleep. When these spaces become enlarged and blocked, the waste accumulates instead of being cleared.
The NTU researchers found that these blockages were linked to four of the seven Alzheimer’s biomarkers they measured, making enlarged perivascular spaces a potentially powerful early indicator. What makes this finding particularly valuable is that these changes are visible on routine MRI — the same type of brain scan that hospitals already perform for headaches, strokes, and other neurological complaints. In other words, radiologists could theoretically flag this finding on scans that are already being done, without requiring expensive PET imaging or spinal fluid analysis. The practical limitation is that most radiologists are not currently trained to look for or report enlarged perivascular spaces in this context. The finding is still making its way from research into clinical practice.
Personality Changes Before Memory Loss — What to Actually Watch For
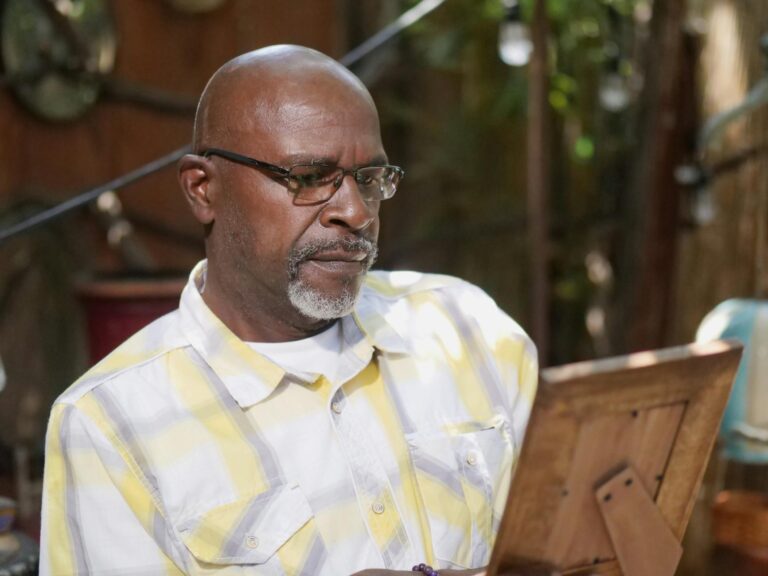
Most people associate dementia with forgetting names and misplacing keys, but research from the UCI MIND center has revealed that personality changes may actually be the first observable sign — not memory loss. Older adults who developed shifts in motivation, patience, humor, or mood were three times more likely to meet criteria for mild cognitive impairment. And once those behavioral changes took hold, cognitive decline progressed more steeply than in people whose personalities remained stable. This is a critical finding because personality changes are often dismissed as normal aging, stress, or depression — and they may go unaddressed for years. The tradeoff here is a difficult one for families.
On one hand, recognizing personality shifts as potential early warning signs could lead to earlier evaluation and intervention. On the other hand, treating every mood change in an aging parent as a sign of dementia would cause unnecessary anxiety and could damage relationships. A father who becomes more irritable in his late 60s might be dealing with chronic pain, sleep problems, or grief — not preclinical Alzheimer’s. The distinguishing factor, according to the research, is the pattern: multiple personality dimensions shifting simultaneously, in ways that are out of character and sustained over months rather than days. A single bad week is not a red flag. A gradual, persistent change in someone’s fundamental temperament — particularly when combined with subtle functional difficulties — warrants a conversation with a neurologist.
Disrupted Brain Connectivity — The Invisible Breakdown
Even before structural damage becomes visible on imaging, the functional connectivity of the brain begins to break down during preclinical Alzheimer’s. According to the Alzheimer’s Association, the balance of neural networks deteriorates, reducing information processing efficiency. Brain regions that normally work in concert start operating more independently, like instruments in an orchestra that gradually lose their ability to follow the conductor. Functional MRI studies have shown that the default mode network — a set of brain regions active during rest, daydreaming, and self-referential thinking — is particularly vulnerable to early disruption in Alzheimer’s.
The warning here is that disrupted connectivity is currently not something a standard clinical visit can detect. Functional MRI is a research tool, not a routine diagnostic test, and interpreting connectivity changes requires specialized software and expertise. There is also significant normal variation in brain connectivity across individuals, which makes it difficult to say with confidence whether a given person’s network function is abnormal or simply at one end of the healthy spectrum. For now, this biomarker is most useful in research settings — helping scientists understand the progression of disease and test whether experimental treatments are restoring network function — rather than as a practical screening tool for individuals.

What the Two-Phase Model Means for Early Detection
The NIH’s two-phase model of Alzheimer’s has practical implications that extend beyond the laboratory. If Phase 1 — the slow, silent accumulation of damage — lasts a decade or more, then there is a substantial window during which interventions might work. The challenge has always been identifying who is in Phase 1 before Phase 2’s rapid destruction begins.
The convergence of blood-based amyloid tests, MRI detection of enlarged perivascular spaces and brain shape changes, and behavioral monitoring for personality shifts gives clinicians more tools than they have ever had. No single test is definitive, but a combination of abnormal findings across these domains paints a compelling picture. For example, a 58-year-old whose routine MRI shows enlarged perivascular spaces, whose family has noticed sustained personality changes over the past year, and whose blood test reveals elevated amyloid-beta would present a very different risk profile than someone with just one of those findings. The multi-biomarker approach is where the field is heading, even if insurance coverage and clinical infrastructure have not caught up yet.
Cognitive Training and the Future of Dementia Prevention
A February 2026 study from Johns Hopkins Medicine added an encouraging piece to the prevention puzzle: cognitive speed training in midlife was linked to lower dementia incidence up to 20 years later. This is not the same as doing crossword puzzles or playing casual brain games. The specific intervention involved structured training designed to improve processing speed — how quickly the brain can take in and respond to information.
The finding suggests that certain types of cognitive exercise may build resilience against the damage accumulating during Phase 1, effectively extending the time before Phase 2 begins. This line of research is still maturing, and it would be premature to claim that any particular app or program will prevent Alzheimer’s. But combined with what we now know about the 15-to-20-year preclinical window, cardiovascular risk management, sleep optimization for glymphatic clearance, and emerging blood-based biomarker tests, the picture is shifting. Dementia prevention is moving from a vague aspiration to a concrete, multi-pronged strategy — one that depends on catching the brain’s earliest changes long before the first memory slips.
Conclusion
The brain changes that precede dementia symptoms are far more varied and far earlier than most people realize. Amyloid-beta accumulation, inhibitory neuron death, myelin damage, immune activation, clogged perivascular spaces, brain shape deformation, disrupted neural connectivity, and personality shifts all unfold during a silent preclinical phase that can last 15 to 20 years. The NIH’s two-phase model makes clear that by the time someone is forgetting conversations or getting lost, the brain has already endured years of quiet destruction — and the rapid second phase is underway. The practical takeaway is that midlife is the critical intervention window.
If you are in your 40s, 50s, or 60s with no cognitive complaints, this is not the time to stop paying attention — it is the time to start. Talk to your doctor about baseline cognitive screening and whether a brain MRI makes sense given your risk profile. Pay attention to sustained personality changes in yourself and your loved ones. Prioritize sleep, cardiovascular health, and structured cognitive engagement. The science is clear that these earliest brain changes are increasingly detectable, and the emerging evidence on prevention — from cognitive speed training to biomarker-guided intervention — suggests that what you do during the silent years genuinely matters.
Frequently Asked Questions
How early can brain changes from Alzheimer’s actually be detected?
In people with genetic risk factors, amyloid plaques have been found forming as early as the late 20s, roughly 15 to 20 years before any cognitive symptoms appear. Blood-based biomarker tests can now detect elevated amyloid-beta years before memory problems begin, and structural MRI can reveal brain shape changes and enlarged perivascular spaces during midlife.
Are personality changes really a sign of early dementia?
Research from UCI MIND found that older adults who developed sustained changes in motivation, patience, humor, or mood were three times more likely to meet criteria for mild cognitive impairment. However, not every personality shift signals dementia — the key is persistent, multi-dimensional change that is out of character, not a temporary bad mood or stressful period.
What are enlarged perivascular spaces and why do they matter?
Perivascular spaces are channels around blood vessels that help clear toxic waste — including amyloid and tau — from the brain. When these spaces become enlarged and clogged, waste accumulates instead of being flushed out. A 2025 study found these blockages are significantly more common in people with mild cognitive impairment and were associated with four of seven Alzheimer’s biomarkers measured.
Can brain games or cognitive training actually prevent dementia?
A February 2026 Johns Hopkins study found that specific cognitive speed training in midlife was linked to lower dementia incidence up to 20 years later. However, this involved structured processing speed exercises, not casual puzzles or games. More research is needed to identify exactly which types of training are most protective.
What is the two-phase model of Alzheimer’s disease?
An NIH study published in October 2024 found that Alzheimer’s damages the brain in two phases. Phase 1 is a long, silent period of slow plaque accumulation, immune activation, myelin damage, and inhibitory neuron loss. Phase 2 is a rapid, destructive phase that coincides with symptom onset and accelerating plaques and tangles. The long duration of Phase 1 represents a potential window for intervention.
Which brain region is affected first in Alzheimer’s disease?
The entorhinal cortex is one of the first regions damaged. It plays a critical role in memory formation and spatial navigation, which is why early behavioral signs can include difficulty with directions or navigation in familiar places. Brain shape changes identified in a UC Irvine study showed that geometric shifts increase this region’s vulnerability.