Alzheimer’s disease is a progressive neurological disorder that affects the brain, leading to memory loss, cognitive decline, and behavioral changes. It is the most common form of dementia, accounting for about 60-80% of all dementia cases. According to the Alzheimer’s Association, over 6 million Americans are living with Alzheimer’s, and this number is expected to rise to nearly 13 million by 2050. With such a significant impact on individuals and their families, it is crucial to understand the criteria for diagnosing Alzheimer’s disease.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a handbook used by mental health professionals to diagnose and classify different mental disorders. The fifth edition of the DSM, known as DSM-5, was published in 2013, and it includes specific criteria for diagnosing Alzheimer’s disease. These criteria are essential in accurately identifying and treating the disease.
The DSM-5 criteria for Alzheimer’s disease are divided into three stages: preclinical, mild cognitive impairment (MCI), and dementia. Each stage has specific requirements that must be met to receive a diagnosis.
Preclinical stage:
The preclinical stage of Alzheimer’s disease refers to the very early phase of the disease when an individual has yet to experience any symptoms. At this stage, changes in the brain have started to occur, but the person is still functioning normally. As such, it can be challenging to detect Alzheimer’s disease during this stage. To be diagnosed with Alzheimer’s in the preclinical stage, an individual must meet several criteria:
1. Presence of abnormal beta-amyloid protein in the brain:
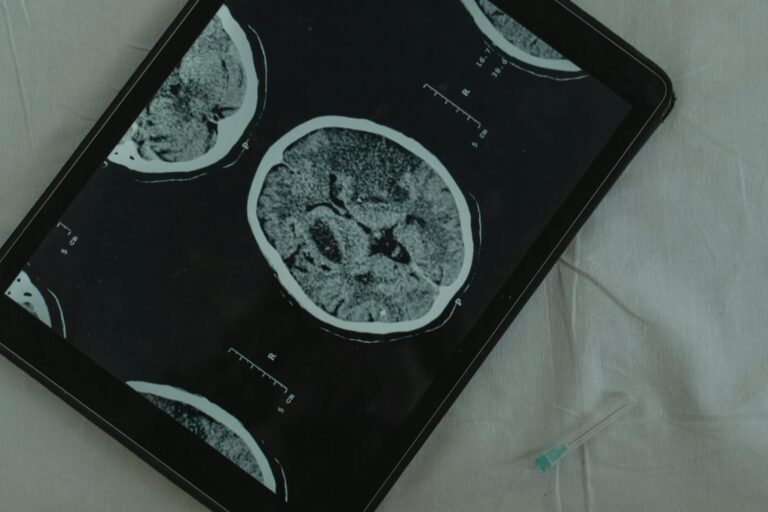
Beta-amyloid is a protein that forms plaques in the brain, which is a hallmark sign of Alzheimer’s disease. In this stage, imaging tests such as PET scans or cerebrospinal fluid (CSF) tests can detect the presence of these plaques.
2. Evidence of neurodegeneration:
Neurodegeneration refers to the progressive loss of brain cells, which is also a characteristic of Alzheimer’s disease. In this stage, imaging tests or CSF tests can detect the presence of neurodegeneration.
3. No evidence of cognitive or functional impairments:
Despite the presence of beta-amyloid and neurodegeneration, an individual in the preclinical stage of Alzheimer’s disease will not show any symptoms or impairments in thinking or daily functioning.
Mild Cognitive Impairment (MCI) stage:
The MCI stage of Alzheimer’s disease is the earliest stage where an individual begins to experience symptoms. These symptoms are not severe enough to interfere with daily activities, but they are noticeable to the individual and their loved ones. To be diagnosed with MCI due to Alzheimer’s disease, an individual must meet the following criteria:
1. Evidence of cognitive decline:
There must be a noticeable decline in cognitive abilities compared to previous levels. This decline may be self-reported or observed by others.
2. Impairment in at least one cognitive domain:
Cognitive domains include memory, language, executive function, attention, and social cognition. In this stage, an individual must have difficulty in at least one of these areas.
3. Preservation of independence in daily activities:
Despite cognitive impairments, an individual in the MCI stage of Alzheimer’s disease can still perform daily tasks independently.
Dementia stage:
The dementia stage of Alzheimer’s disease is the most advanced stage, characterized by significant memory loss, impaired thinking and reasoning, and difficulty performing daily tasks. To be diagnosed with Alzheimer’s dementia, an individual must meet the following criteria:
1. Evidence of significant cognitive decline:
There must be a noticeable decline in cognitive abilities compared to previous levels. This decline may be self-reported or observed by others.
2. Impairment in at least two cognitive domains:
In this stage, an individual must have difficulty in at least two cognitive domains, including memory, language, executive function, attention, and social cognition.
3. Significant interference with daily activities:
The cognitive impairments must be severe enough to interfere with daily activities, such as managing finances, driving, or personal hygiene.
4. Not due to other conditions:
Other medical conditions, such as medication side effects or other types of dementia, must not be the primary reason for the cognitive decline.
It is essential to note that these criteria are not a one-size-fits-all approach. Each individual’s experience with Alzheimer’s disease may be different, and the progression of the disease may vary. These criteria serve as guidelines for mental health professionals to make an accurate diagnosis and provide appropriate treatment.
In conclusion, the DSM-5 criteria for Alzheimer’s disease outline the specific requirements for diagnosing the disease at various stages. An accurate diagnosis is crucial in managing symptoms, providing appropriate care, and planning for the future. If you or a loved one are experiencing memory loss or other symptoms of Alzheimer’s disease, it is essential to talk to a healthcare professional for proper evaluation and treatment. While there is currently no cure for Alzheimer’s disease, early diagnosis and intervention can help improve the quality of life for individuals and their families.