Dementia progression in younger patients — typically those diagnosed before age 65 — tends to be faster, more aggressive, and more varied in its symptoms compared to late-onset cases. While older adults with Alzheimer’s disease often experience a gradual decline centered on memory loss, younger patients frequently present with unusual symptoms first, such as difficulty finding words, problems with visual processing, or personality changes that get misdiagnosed as depression or burnout. A 52-year-old architect, for instance, might notice she can no longer read blueprints or judge spatial relationships months before any memory problems surface, a pattern that would be uncommon in someone diagnosed at 78.
Beyond the speed of decline, younger-onset dementia differs in the types of dementia involved, the genetic factors at play, and the broader life disruption it causes. Someone in their 40s or 50s is likely still working, possibly raising children, and carrying a mortgage — realities that fundamentally change how the disease is experienced and managed. This article covers how and why progression differs by age, which forms of dementia are more common in younger patients, what the research says about rate of cognitive decline, and what practical steps families and patients can take when facing a diagnosis that arrives decades earlier than expected.
Table of Contents
- Why Does Dementia Progress Differently in Younger Patients?
- Which Types of Dementia Are More Common in Younger Adults?
- The Role of Genetics in Younger-Onset Dementia
- Managing Daily Life When Dementia Strikes During Working Years
- Behavioral and Psychiatric Symptoms in Younger Patients
- How Physical Health Intersects With Younger-Onset Decline
- Research Momentum and the Outlook for Younger Patients
- Conclusion
- Frequently Asked Questions
Why Does Dementia Progress Differently in Younger Patients?
The leading explanation for faster progression in younger-onset dementia is that the underlying disease biology often differs from what occurs in older adults. In late-onset Alzheimer’s, the most common form, the disease is driven largely by a slow accumulation of amyloid plaques and tau tangles over decades, compounded by age-related vascular damage and inflammation. In younger patients, the pathology tends to be more purely neurodegenerative — less muddied by other aging processes but also more aggressive in how it attacks specific brain networks. Research published in the journal *Neurology* has found that younger Alzheimer’s patients show more widespread tau pathology at diagnosis compared to older patients at a similar clinical stage, which may help explain the faster trajectory. There is also a diagnostic factor that complicates the picture. Because no one expects a 48-year-old to have dementia, symptoms are often attributed to stress, anxiety, or midlife depression for a year or more before the correct diagnosis is reached.
By the time a younger patient receives a formal diagnosis, they may already be at a more advanced stage than the clinical label suggests. This diagnostic delay does not change the biology, but it compresses the perceived timeline. A patient’s family may feel the decline is shockingly rapid when in reality the disease had a longer undetected runway. It is worth noting that not all younger patients progress quickly. Some forms of young-onset dementia, particularly certain frontotemporal variants, can have a relatively slow course spanning a decade or more. Generalizations about speed are useful but should never replace individual clinical assessment. A neurologist tracking biomarkers and cognitive testing over time provides a far more accurate picture than any statistical average.
Which Types of Dementia Are More Common in Younger Adults?
Alzheimer’s disease still accounts for the largest share of younger-onset dementia, representing roughly 30 to 40 percent of cases. However, the proportion shifts significantly compared to late-onset populations. Frontotemporal dementia, which is rare in people over 75, is one of the most common causes of dementia in people under 60. Vascular dementia, dementia with lewy bodies, and alcohol-related brain damage also appear at notable rates. Rarer causes like Huntington’s disease, Creutzfeldt-Jakob disease, and autoimmune encephalitis make up a larger slice of the pie in younger cohorts simply because they tend to strike earlier in life. The type of dementia matters enormously for progression.
Frontotemporal dementia affecting behavior — known as the behavioral variant — may leave memory relatively intact for years while profoundly altering personality, impulse control, and social awareness. A previously reserved accountant might begin making inappropriate comments at work, spending recklessly, or losing all interest in personal hygiene. This is not Alzheimer’s with a different name; it is a different disease attacking different brain regions, and its progression follows a different map. However, if a younger patient is diagnosed with Alzheimer’s specifically, research from the Mayo Clinic and other centers suggests their cognitive decline may actually be steeper year-over-year than in an older patient with the same diagnosis. One important limitation of this research is that most longitudinal studies rely on standardized cognitive tests that may not capture the particular deficits younger patients experience, such as executive function problems or visuospatial difficulties that standard memory-focused assessments can miss. Families should push for comprehensive neuropsychological testing that goes beyond simple memory screening.
The Role of Genetics in Younger-Onset Dementia
Genetics plays a larger role in younger-onset dementia than in late-onset cases, though the relationship is more nuanced than many families expect. Truly hereditary, deterministic mutations — the kind where inheriting the gene virtually guarantees developing the disease — account for only about 10 to 15 percent of young-onset Alzheimer’s cases. These involve mutations in genes like APP, PSEN1, and PSEN2, and they tend to cause onset in the 30s, 40s, or early 50s. A family in Antioquia, Colombia, carrying the PSEN1 E280A mutation has been extensively studied; affected members reliably develop symptoms around age 44, and the progression follows a predictable, aggressive course that has made this population invaluable for drug trials.
For the majority of younger patients without a deterministic mutation, the genetic picture is murkier. Carrying one or two copies of the APOE4 allele raises risk and is associated with earlier onset, but it does not guarantee disease and does not reliably predict how fast someone will decline. Many younger patients and their families pursue genetic testing hoping for clear answers and instead receive probabilistic information that requires careful genetic counseling to interpret. Genetic testing is most useful when there is a clear family pattern of multiple members developing dementia before age 60, which can suggest one of the autosomal dominant mutations worth identifying for the sake of the patient and their biological relatives.
Managing Daily Life When Dementia Strikes During Working Years
The practical fallout of a dementia diagnosis at 50 is categorically different from one at 80, and management strategies need to reflect this. A younger patient may still be the primary earner for a household with dependents. They may have a mortgage with 20 years remaining, children in school, and a spouse who is also working full-time. The immediate priority after diagnosis shifts to financial and legal planning — establishing power of attorney, reviewing disability insurance, contacting Social Security about SSDI eligibility, and understanding how quickly workplace accommodations may become insufficient. There is a genuine tradeoff in how much to disclose and how early. Some younger patients benefit from telling their employer promptly, particularly in safety-sensitive roles, while others in more flexible positions may choose to manage symptoms quietly for a period to preserve income and insurance.
Neither approach is universally correct. The calculus depends on the type of work, the employer’s culture, the patient’s current symptom severity, and the legal protections available. An employment attorney familiar with the Americans with Disabilities Act can help families navigate this. Compared to older patients who may transition from independent living to assisted living along a well-trodden path, younger patients face a gap in the care system. Most adult day programs and memory care facilities are designed for people in their 70s and 80s. A 55-year-old placed in a facility geared toward much older residents often finds the environment unstimulating and socially isolating. Some regions have developed younger-onset-specific programs, but they remain uncommon, and families frequently end up cobbling together support from a mix of home care aides, community resources, and their own time.
Behavioral and Psychiatric Symptoms in Younger Patients
Behavioral and psychiatric symptoms deserve special attention in younger-onset dementia because they tend to appear earlier in the disease course and can be more severe. Depression, anxiety, apathy, agitation, and psychosis all occur at higher rates in younger patients compared to older ones at the same disease stage. In frontotemporal dementia, behavioral changes are often the defining feature, but even in younger-onset Alzheimer’s, psychiatric symptoms are more prominent than families typically expect. A significant warning for caregivers and clinicians: these behavioral symptoms are frequently the initial presenting complaint, which means they get treated as primary psychiatric conditions. A 47-year-old woman with early frontotemporal dementia may receive a diagnosis of bipolar disorder and be prescribed mood stabilizers for two years before anyone suspects a neurodegenerative cause.
Antidepressants and antipsychotics may partially manage symptoms but will not address the underlying progression, and some medications — particularly anticholinergics — can worsen cognitive function. Any psychiatric presentation with an atypical course or poor medication response in a middle-aged patient should prompt a neurology referral and neuroimaging. The emotional toll on caregiving spouses is also distinct. Caring for a partner with dementia at 50 means potentially decades of caregiving ahead, loss of the partnership during years that were expected to be active and shared, and a social circle that often does not understand the situation. Younger caregivers report higher rates of depression and financial strain than older caregivers, and they have fewer peers going through the same experience. Connecting with organizations like the Association for Frontotemporal Degeneration or the Alzheimer’s Association’s younger-onset support groups can be genuinely helpful, though these resources are not available in every community.

How Physical Health Intersects With Younger-Onset Decline
Younger patients generally enter the disease with better cardiovascular and overall physical health than older patients, which creates a paradox: their bodies remain relatively strong even as cognition deteriorates. A 55-year-old with moderate dementia may still be physically capable of driving, leaving the house unsupervised, or operating kitchen appliances — activities that become safety risks well before the patient recognizes the danger.
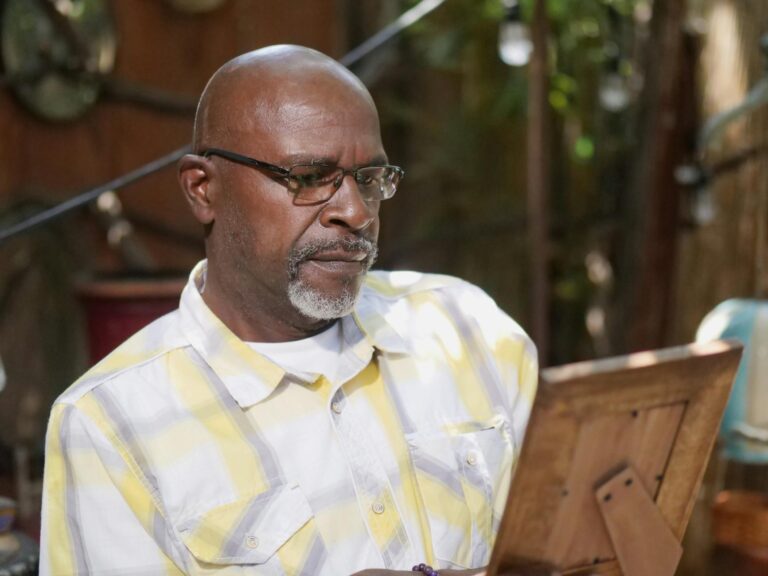
One family reported that their 58-year-old father with Alzheimer’s continued his daily five-mile run for two years after diagnosis, which was excellent for his physical health but created real anxiety because he occasionally became disoriented during the route and could not find his way home. This physical-cognitive mismatch means that safety planning needs to happen earlier and more explicitly than families anticipate. Driving assessments, home safety modifications, and GPS tracking strategies become relevant at a point when the patient often still looks and feels healthy, which can make these conversations feel premature and provoke resistance.
Research Momentum and the Outlook for Younger Patients
The research landscape for younger-onset dementia has shifted considerably in recent years. The approval of anti-amyloid therapies like lecanemab and donanemab, while primarily studied in early Alzheimer’s populations that include many younger patients, represents the first disease-modifying treatments rather than purely symptomatic ones. Younger patients with confirmed amyloid pathology are often considered strong candidates for these therapies because they tend to have fewer comorbidities that complicate treatment and their brains may have more capacity to benefit from slowing the disease early.
Clinical trials are also increasingly recruiting younger cohorts and studying presymptomatic carriers of genetic mutations, which means the very population most affected by young-onset Alzheimer’s is now at the center of prevention research. Families dealing with a younger-onset diagnosis today should ask their neurologist about clinical trial eligibility. The Dominantly Inherited Alzheimer Network, the Alzheimer’s Prevention Initiative, and trial matching services through the Alzheimer’s Association can connect patients with studies that may offer access to emerging treatments years before they reach the general market.
Conclusion
Dementia in younger patients is not simply the same disease arriving early. It progresses differently — often faster, with a wider range of initial symptoms, greater genetic involvement, and a fundamentally different impact on daily life. The types of dementia shift toward frontotemporal and atypical Alzheimer’s variants, behavioral symptoms are more prominent, and the care system is poorly designed for someone decades younger than the typical patient.
Understanding these differences is not academic; it directly affects how quickly the diagnosis is made, how the disease is managed, and what support the patient and family need. For anyone facing a younger-onset diagnosis, the priorities are clear: get a thorough diagnostic workup including neuroimaging and neuropsychological testing, address financial and legal planning immediately, connect with younger-onset-specific support networks, and ask about clinical trial participation. The research trajectory is more promising than it has ever been, but the current reality still demands that families be proactive, informed, and willing to advocate aggressively within a healthcare system that too often fails to recognize dementia in someone who does not look old enough to have it.
Frequently Asked Questions
At what age is dementia considered “younger-onset”?
The standard cutoff is diagnosis before age 65, though some researchers use 60. The term applies regardless of the type of dementia. Symptoms may begin years before the formal diagnosis, so a person diagnosed at 63 may have first noticed problems at 58 or 59.
Is younger-onset dementia always inherited?
No. While genetics play a larger role than in late-onset cases, the majority of younger-onset dementia is not caused by a single inherited gene mutation. Only about 10 to 15 percent of young-onset Alzheimer’s cases involve deterministic autosomal dominant mutations. Most cases involve a combination of genetic risk factors and other biological processes.
How long can someone live with younger-onset dementia?
This varies widely by dementia type and individual factors. Young-onset Alzheimer’s may progress over 7 to 12 years from diagnosis, though some patients live longer. Certain frontotemporal dementia variants can span a decade or more, while rarer conditions like Creutzfeldt-Jakob disease progress over months. Physical health at the time of diagnosis significantly influences survival.
Can younger patients with dementia still work?
Many can continue working for a period after diagnosis, particularly in roles that can be modified or that do not involve safety-critical decisions. The duration depends on the type of dementia, the specific symptoms, and the nature of the work. Some patients work productively for a year or more with appropriate accommodations, while others need to stop relatively quickly.
Should children of younger-onset dementia patients get genetic testing?
This is a deeply personal decision best made with the guidance of a genetic counselor. Testing is most informative when the affected parent has a known deterministic mutation. If the parent’s genetic status is unknown, testing the children may produce ambiguous results. Adult children should understand what they want to do with the information before pursuing testing, as results cannot be unknown.
Are the new Alzheimer’s drugs effective for younger patients?
Anti-amyloid therapies like lecanemab have shown modest slowing of decline in early-stage Alzheimer’s patients, and younger patients with confirmed amyloid pathology are generally considered good candidates. However, these drugs carry risks including brain swelling and microbleeds, particularly in APOE4 carriers. They also do not work for non-Alzheimer’s dementias. Eligibility and risk-benefit should be discussed with a neurologist familiar with these treatments.