A neuropsychological evaluation for dementia is a structured, multi-hour assessment conducted by a licensed neuropsychologist that measures how well different regions of the brain are functioning — not by imaging them directly, but by testing the cognitive abilities they control. The evaluation maps a person’s relative strengths and weaknesses across domains like memory, attention, language, processing speed, visuospatial skills, and executive function. From that profile, a trained clinician can determine whether a person’s cognition falls within normal aging, meets criteria for mild cognitive impairment (MCI), or reflects a specific dementia syndrome.
In the right hands, the process can distinguish Alzheimer’s disease from non-dementia with nearly 90% accuracy. For a family member watching a parent repeat the same question three times at dinner, the evaluation is often the first rigorous step toward understanding what’s happening. It replaces guesswork with data. This article covers how the process unfolds from start to finish, what the tests actually measure, how long it takes, what it costs, and what the results can — and cannot — tell you.
Table of Contents
- What Happens During a Neuropsychological Evaluation for Dementia?
- Which Cognitive Domains Are Tested, and Why Do They Matter?
- What Conditions Can a Neuropsychological Evaluation Detect?
- How Long Does a Neuropsychological Evaluation Take, and What Does It Cost?
- How Accurate Is Neuropsychological Testing for Dementia Diagnosis?
- When Should Someone Be Re-Evaluated, and How Is Follow-Up Structured?
- How Is the Field of Neuropsychological Assessment Evolving?
- Conclusion
- Frequently Asked Questions
What Happens During a Neuropsychological Evaluation for Dementia?
The evaluation begins well before any formal testing. A licensed neuropsychologist conducts a clinical interview that covers the person’s full medical history, educational background, occupational history, and current cognitive concerns. This intake also typically includes a family member or close caregiver acting as an informant — someone who can describe changes they’ve observed over time, since people with early dementia often lack full awareness of their own deficits. A spouse might report that their partner has stopped managing the household finances or has become uncharacteristically withdrawn, details the patient may not volunteer or even notice.
Following the interview, the formal testing begins. The neuropsychologist administers a battery of standardized written and oral tests designed to probe specific cognitive systems. These include attention and working memory tasks like the WMS-IV Digit Span, processing speed tests like the Trail Making Test Part A and the WAIS-IV Symbol Search, episodic memory tasks, language assessments, and executive function measures. Each test has population-level norms, so a person’s performance is compared to others of the same age and education level — making it possible to distinguish a low score caused by limited schooling from one caused by neurological decline.

Which Cognitive Domains Are Tested, and Why Do They Matter?
The six core domains assessed in a standard neuropsychological evaluation each correspond to specific neural networks. Attention and processing speed reflect the integrity of frontal-subcortical circuits. Episodic memory — the ability to learn and recall new information — is primarily mediated by the hippocampus and surrounding medial temporal structures, the areas hit earliest and hardest in Alzheimer’s disease. Language testing can reveal word-finding difficulties and naming deficits. Visuospatial tasks probe posterior cortical function.
Executive function tests, which assess planning, cognitive flexibility, and impulse control, implicate the prefrontal cortex. Research has identified episodic memory and executive function as the two strongest predictors of a person’s daily functional capacity — meaning how well they can manage real-world tasks independently. This is why those domains receive particular emphasis. However, the profile across all domains matters as much as any single score. A person who shows profound memory impairment but intact executive function has a different clinical picture than someone with the opposite pattern, and those differences point toward different diagnoses and different disease trajectories. A single low score in isolation rarely means much; the full pattern does.
What Conditions Can a Neuropsychological Evaluation Detect?
One of the most clinically important uses of neuropsychological evaluation is distinguishing between types of dementia — a task that standard screening tools like the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA) are poorly equipped to handle. A brief office screening might flag general impairment without revealing whether it reflects Alzheimer’s disease, vascular dementia, Lewy body dementia, or a less common syndrome. Neuropsychological evaluation is particularly valuable for detecting atypical dementia syndromes that are frequently missed in general clinical settings.
Primary progressive aphasia, for example, presents primarily as a language breakdown rather than memory loss — patients may struggle to find words or lose the ability to produce fluent speech while remaining socially engaged and oriented. Behavioral variant frontotemporal dementia (bvFTD) often begins with personality changes, social disinhibition, or apathy rather than forgetfulness, and is commonly misdiagnosed as depression or a psychiatric condition before the cognitive picture clarifies. Posterior cortical atrophy affects visual processing and spatial reasoning, leading to trouble reading, driving difficulty, or problems recognizing faces, while episodic memory may remain relatively preserved in early stages. Without comprehensive neuropsychological testing, all three of these conditions can go unrecognized for years.

How Long Does a Neuropsychological Evaluation Take, and What Does It Cost?
A typical neuropsychological evaluation takes between four and eight hours of direct testing time, though more focused referrals may require only two to five hours. That testing time represents only part of the total professional investment. Complex evaluations can involve 15 to 25 hours of total professional time when scoring, interpretation, and report writing are included — a labor-intensive process that explains much of the cost. Without insurance, a neuropsychological evaluation typically runs between $1,500 and $7,000 or more.
In major metropolitan areas the figures skew higher: in Los Angeles, for example, costs commonly range from $3,000 to $6,000. Most private insurance plans and Medicaid provide some coverage when the evaluation is deemed medically necessary, but coverage varies substantially by plan, and prior authorization is often required. The comparison worth making here is between the cost of evaluation and the cost of delayed or incorrect diagnosis — wrong dementia diagnoses lead to inappropriate medications, missed treatment windows, and inadequate care planning. For families weighing the expense, the evaluation’s role in shaping years of downstream care decisions puts the upfront cost in different context.
How Accurate Is Neuropsychological Testing for Dementia Diagnosis?
Neuropsychological testing performs well compared to other diagnostic methods, particularly for distinguishing Alzheimer’s dementia from normal cognition. Studies show accuracy approaching 90% for that specific distinction. For predicting whether a person with current impairment will progress to dementia, neuropsychological profiles show predictive accuracy ranging from roughly 80% to 100%, with sensitivities between 53% and 80% and specificities between 67% and 99%. Those ranges reflect an important caveat: no single diagnostic tool, including neuropsychological evaluation, is infallible.
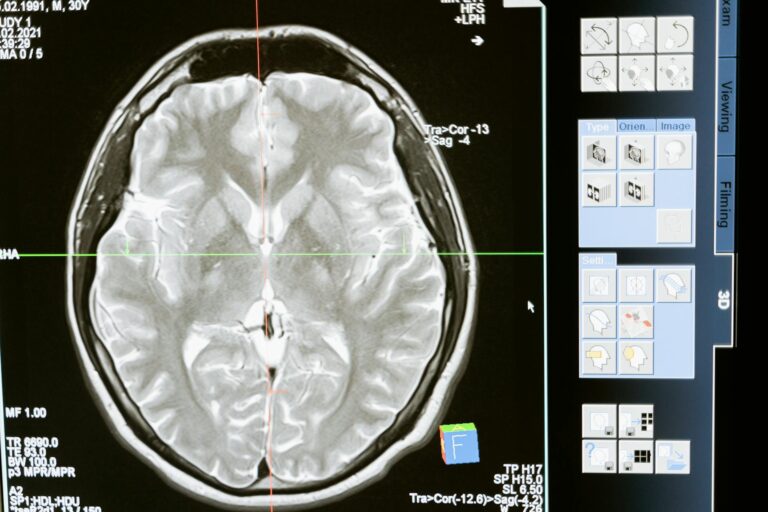
Sensitivity and specificity vary depending on the specific condition being tested, the population studied, and the criteria used. Factors like test-taking anxiety, pain, fatigue, depression, and medication effects can artificially depress scores and lead to overestimation of impairment. A skilled neuropsychologist accounts for these factors in interpretation, but they cannot always be fully disentangled from genuine cognitive decline. This is why evaluation results are interpreted in the context of the full clinical picture — neuroimaging, laboratory findings, medical history — rather than as standalone verdicts.

When Should Someone Be Re-Evaluated, and How Is Follow-Up Structured?
Neuropsychological evaluation is not always a one-time event. When testing reveals abnormalities, a follow-up evaluation in one year is generally recommended to track whether impairment is stable, improving, or progressing. Progression across serial evaluations is diagnostically informative in its own right — stable impairment after a stroke follows a different trajectory than the slow, continuous decline typical of Alzheimer’s disease.
For individuals who test within normal limits but carry known risk factors — a strong family history, subjective cognitive complaints not yet reflected in formal scores, or evidence of early biomarker changes — re-evaluation in two years is the standard recommendation. This follow-up structure reflects the field’s understanding that neuropsychological testing captures a snapshot; the longitudinal picture often tells the fuller story. A 68-year-old who scores in the low-normal range today and shows measurable decline two years later has provided clinically important data that a single evaluation could never yield.
How Is the Field of Neuropsychological Assessment Evolving?
The field is not standing still. A 2025 paper in Alzheimer’s & Dementia by Shaughnessy and colleagues reaffirmed the central role of neuropsychological assessment in evaluating patients with suspected Alzheimer’s disease and related dementias, underscoring its continued relevance even as new biomarker-based diagnostic tools emerge. Simultaneously, a 2025 review in Frontiers in Human Neuroscience is actively rethinking how traditional neuropsychological tests should be validated in an era of neuroimaging and digital biomarkers — recognizing that the gold standards themselves may need updating.
The direction the field appears to be moving is toward integration rather than replacement. Digital cognitive testing platforms, blood-based biomarkers like phosphorylated tau and amyloid ratios, and advanced neuroimaging are becoming increasingly available, and the most rigorous diagnostic approaches will likely combine these tools with comprehensive neuropsychological assessment rather than substitute one for the other. The human clinician interpreting a full cognitive profile — accounting for education, culture, emotional state, and test behavior — brings something that a biomarker panel alone cannot provide.
Conclusion
A neuropsychological evaluation for dementia works by systematically measuring how the brain performs across the cognitive domains it controls — attention, memory, language, processing speed, visuospatial processing, and executive function — and comparing those measurements against age- and education-adjusted norms. The process begins with a clinical interview, moves through four to eight hours of standardized testing, and concludes with a detailed report that maps cognitive strengths and weaknesses, differentiates between dementia syndromes, and guides treatment planning and care decisions.
For families navigating a loved one’s memory concerns, or for individuals tracking their own cognitive health, a neuropsychological evaluation represents the most thorough available window into brain function short of direct imaging or tissue analysis. It is not infallible, and it works best as part of a complete clinical workup rather than in isolation. But for conditions that standard screening tools routinely miss — atypical dementias, early MCI, subtle executive decline — it remains one of the most valuable diagnostic tools available.
Frequently Asked Questions
Is a neuropsychological evaluation the same as a cognitive screening test?
No. A cognitive screening test like the MoCA or MMSE takes 10 to 15 minutes and provides a rough pass/fail signal. A neuropsychological evaluation takes four to eight hours, measures dozens of specific cognitive functions, and produces a detailed diagnostic profile. Screenings are useful for flagging that something may be wrong; evaluations are designed to explain what it is.
Does a person need a referral to get a neuropsychological evaluation?
In most cases, yes — either from a primary care physician or a specialist like a neurologist or psychiatrist. Insurance coverage almost always requires a referral and a determination of medical necessity. Some private neuropsychology practices accept self-referrals, but out-of-pocket costs apply.
Can anxiety or depression affect the results?
Yes, significantly. Depression in particular can cause slowed processing speed and memory difficulties that mimic early dementia — a pattern sometimes called pseudodementia. A skilled neuropsychologist incorporates mood assessment into the evaluation and considers emotional state when interpreting scores, but this remains one of the more challenging aspects of differential diagnosis.
How should someone prepare for a neuropsychological evaluation?
Get a full night of sleep, take regular medications as prescribed, bring glasses and hearing aids if applicable, and eat before the appointment. Fatigue and sensory impairment can meaningfully depress scores. There is no specific studying or preparation that helps — the tests are designed to measure current function, not acquired knowledge.
Will the neuropsychologist diagnose dementia on the same day?
Usually not. Testing data must be scored, interpreted, and written into a report — a process that typically takes one to several weeks. A feedback session is then scheduled to review findings with the patient and family. Some practices offer a brief preliminary summary at the end of testing, but the formal diagnosis comes with the written report.
Can a neuropsychological evaluation be done virtually?
Partially. Some standardized tests have been adapted for remote administration, and telehealth neuropsychology expanded significantly after 2020. However, certain visuospatial, motor, and hands-on tests require in-person administration, so fully remote evaluations have limitations. Hybrid models combining remote interview and in-person testing are increasingly common.