For a person diagnosed with dementia at age 70, the average lifespan is roughly 7 to 10 years beyond diagnosis, though this range shifts meaningfully depending on the type of dementia, the patient’s sex, and their overall health. A woman diagnosed at 70 tends to fall toward the higher end of that range, while a man of the same age may have closer to 5 to 7 years. These are not fixed numbers carved into stone. They are statistical midpoints drawn from large populations, and individual experiences diverge from them constantly. Consider two 70-year-old men diagnosed with dementia in the same year: one with early-stage Alzheimer’s and no major cardiovascular disease might live another decade, while another with vascular dementia and diabetes might decline within four or five years. What makes these figures especially relevant now is a landmark 2025 BMJ study that analyzed 261 longitudinal studies covering 5,553,960 people with dementia.
That research found that a diagnosis at age 65 reduces life expectancy by approximately 13 years, while a diagnosis at age 80 reduces it by only 3 to 4 years. The takeaway for a 70-year-old falls somewhere between those markers, and the data offers the most robust picture we have had to date. This article breaks down the survival statistics by dementia type, explains why sex and ethnicity influence outcomes, identifies the factors families should watch for, and provides practical guidance for planning after a diagnosis. A dementia diagnosis at 70 also arrives at a particular moment in a person’s life. Many people at that age are still physically active, socially engaged, and living independently. The diagnosis does not erase all of that overnight. Understanding the realistic timeline helps families plan for care needs, legal and financial arrangements, and the kinds of daily life adjustments that become necessary as the disease progresses.
Table of Contents
- How Long Does a Person Live After a Dementia Diagnosis at Age 70?
- Why Dementia Type Changes the Survival Outlook Significantly
- How Sex, Ethnicity, and Health Shape Individual Outcomes
- Planning for the Years Ahead After a Diagnosis at 70
- Why Averages Can Be Misleading for Individual Families
- The Scale of Dementia in the United States in 2025
- What Emerging Research Means for Future Diagnoses
- Conclusion
- Frequently Asked Questions
How Long Does a Person Live After a Dementia Diagnosis at Age 70?
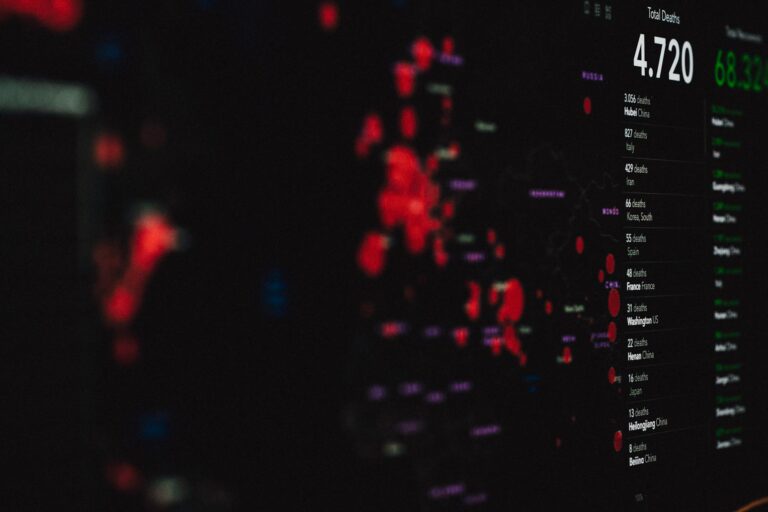
The most commonly cited figure is 7 to 10 years of survival after a dementia diagnosis in the late 60s to early 70s, and the data behind that estimate is substantial. According to the Alzheimer’s Association, patients diagnosed in their 60s and early 70s can expect a median lifespan of 7 to 10 years post-diagnosis. The BrightFocus Foundation and AgeSpace report similar ranges, with Alzheimer’s disease specifically offering approximately 7 additional years for those diagnosed between ages 70 and 79. These figures represent medians and averages, meaning that roughly half of patients live longer and half live shorter than the stated number. The 2025 BMJ systematic review adds considerable depth to these estimates. That study, the largest of its kind, found that 90 percent of dementia patients were still alive one year after diagnosis, but only 21 percent survived to the 10-year mark. For someone diagnosed at 70, that means the overwhelming majority will live well beyond the first year or two, but the probability of reaching the decade mark is roughly one in five.
The study also confirmed what clinicians have long observed: women live approximately 20 percent longer than men after a dementia diagnosis. Women diagnosed at age 60 averaged 9 years of survival, while men diagnosed at the same age averaged 6.5 years. By age 85, those numbers drop to 4.5 years for women and just over 2 years for men. Comparing these numbers to the general population puts the loss in sharper focus. The Alzheimer’s Association reports that at age 70, individuals with Alzheimer’s disease are twice as likely to die before age 80 compared to those without the disease. That doubling of mortality risk is not abstract. It means that a healthy 70-year-old might reasonably expect to live into their mid-to-late 80s, while a 70-year-old with dementia will more likely die in their late 70s or early 80s, though some will exceed those expectations.

Why Dementia Type Changes the Survival Outlook Significantly
Not all dementias behave the same way, and the type of dementia a person has at 70 is one of the most significant variables in how long they will live. Alzheimer’s disease, the most common form, carries an average survival of 8 to 12 years and tends to progress more slowly than other types. The 2025 BMJ review found that Alzheimer’s patients lived approximately 1.4 years longer on average than those with other dementia subtypes. Vascular dementia, the second most common form, has a considerably shorter average survival of about 4 years, largely because it is driven by the same cardiovascular damage that causes strokes and heart disease. Lewy body dementia falls somewhere in the middle, with an average survival of 5 to 7 years, though the range is enormous, stretching from 2 years to as many as 20.
That wide range reflects the unpredictable nature of Lewy body dementia, which can present with severe motor symptoms early or remain primarily cognitive for years. frontotemporal dementia generally carries a shorter prognosis than Alzheimer’s, though it tends to strike at younger ages, which complicates direct comparisons. However, there is a critical limitation families should understand: many people receive a general “dementia” diagnosis without a specific subtype identified, particularly in primary care settings without access to advanced imaging or specialist evaluation. If your loved one was diagnosed at 70 with “dementia” but no one has clarified whether it is Alzheimer’s, vascular, Lewy body, or something else, the survival estimates you read online may not apply cleanly. Pushing for a more specific diagnosis through a neurologist, neuropsychological testing, or imaging can help clarify the likely trajectory and allow for more targeted treatment and planning.
How Sex, Ethnicity, and Health Shape Individual Outcomes
The statistical averages tell one story, but individual outcomes depend heavily on factors that vary from person to person. Sex is one of the most powerful modifiers. Women consistently outlive men after a dementia diagnosis by a margin of roughly 20 percent. This mirrors the broader life expectancy gap between men and women, but it persists even after accounting for the fact that women are diagnosed with dementia more frequently. Almost two-thirds of Americans with Alzheimer’s are women, according to the Alzheimer’s Association’s 2025 data, so the disease disproportionately affects women both in prevalence and in the years they spend living with it. Ethnicity also appears to influence survival.
The 2025 BMJ review found that Asian populations showed survival up to 1.4 years longer than other populations studied. The reasons behind this are not fully understood and likely involve a combination of genetic factors, dietary patterns, social structures, and differences in healthcare access and diagnosis timing. Researchers caution against drawing simple conclusions from this finding, as diagnosis practices and healthcare systems vary dramatically across countries and cultures. Consider a specific example: a 70-year-old woman in good cardiovascular health with early-stage Alzheimer’s and strong family support might realistically live 10 or more years after diagnosis. Compare that to a 70-year-old man with vascular dementia, poorly controlled diabetes, and limited social engagement, whose prognosis might be closer to 3 to 5 years. The diagnosis itself matters, but the context around it matters just as much. Comorbidities such as heart disease, diabetes, and chronic lung disease accelerate decline, while physical fitness, cognitive engagement, and social connection appear to slow it, at least modestly.
Planning for the Years Ahead After a Diagnosis at 70
Once the survival statistics are understood in broad strokes, the practical question becomes: how should a family use this information? A 7-to-10-year horizon is long enough that significant planning is both possible and necessary, but short enough that urgency matters. The first year after diagnosis is typically the best window for making legal, financial, and care decisions, because the diagnosed person can still participate meaningfully in those conversations. Families face a real tradeoff between planning for the long end of the range and the short end. If you plan only for 4 or 5 years and your loved one lives 10, you may run out of financial resources or care arrangements. If you plan for 12 years and the disease progresses quickly, you may have spent time and money on preparations that were never needed. A reasonable approach is to plan financially for the longer end of the estimate while establishing care plans that can be adjusted as the disease progresses.
Long-term care insurance, if available, becomes extremely valuable in this context. The Alzheimer’s Association projects that health and long-term care costs for dementia patients will reach $384 billion in the United States in 2025, and individual families bear a substantial portion of that burden. The comparison between home care and facility-based care also becomes relevant on this timeline. Many families start with home care in the early and middle stages, then transition to memory care facilities as the disease advances. That transition typically happens 3 to 5 years after diagnosis, but it varies enormously depending on the rate of progression, the availability of family caregivers, and the financial resources at hand. Having the conversation about what that transition would look like before it becomes urgent gives everyone involved more control over the process.
Why Averages Can Be Misleading for Individual Families
The most important caveat about all of these statistics is that they describe populations, not individuals. The 2025 BMJ study found that while 90 percent of dementia patients survived one year, only 21 percent reached 10 years. That is an enormous spread, and it means that a 70-year-old receiving a diagnosis today could reasonably fall anywhere within that range. Families who anchor too firmly on a single number, whether it is the optimistic end or the pessimistic end, can find themselves unprepared for the reality that unfolds. Stage at diagnosis is a particularly important variable that published averages often fail to capture. A person diagnosed at 70 during a routine cognitive screening, when symptoms are still mild, has a different trajectory than someone diagnosed at 70 after a crisis event like getting lost or a serious fall, which may indicate more advanced disease.
The average survival figures blend these populations together, making them less useful for any one person’s specific situation. If the diagnosis comes early, survival from the point of diagnosis will naturally be longer, but that does not mean the disease itself is progressing more slowly. There is also the matter of what “survival” means in lived terms. The later years of a 10-year survival period look very different from the early years. A person may be functionally independent for 3 to 5 years, need moderate assistance for another 2 to 3 years, and require full-time care for the final stretch. Families should plan not just for how many years remain, but for what those years will look like at each stage, and what kind of support will be needed as independence diminishes.

The Scale of Dementia in the United States in 2025
The individual experience of a dementia diagnosis at 70 plays out against a backdrop of staggering national numbers. The Alzheimer’s Association estimates that 7.2 million Americans aged 65 and older are living with Alzheimer’s dementia in 2025, with 74 percent of them age 75 or older.
The projected $384 billion in health and long-term care costs reflects a healthcare system that is already straining under the weight of an aging population, and those costs are expected to climb as the baby boomer generation moves deeper into the highest-risk age brackets. For a family navigating a new diagnosis, these macro-level numbers translate into very practical realities: long wait times for specialist appointments, limited availability of memory care beds in some regions, and a caregiver workforce that is stretched thin. Understanding that the system is under pressure can help families act with appropriate urgency in securing resources, rather than assuming that help will be easily available whenever they need it.
What Emerging Research Means for Future Diagnoses
The landscape of dementia care is shifting, though slowly. New anti-amyloid therapies approved in recent years offer the first disease-modifying treatments for Alzheimer’s, though their effects on survival are still being studied and their benefits appear modest so far. Blood-based biomarker tests are making earlier and more accurate diagnosis possible, which could change survival statistics in the coming years by shifting the point of diagnosis earlier in the disease course.
For someone diagnosed at 70 today, these advances may or may not change their personal trajectory. But they do suggest that the survival figures we rely on now, drawn from populations diagnosed in earlier eras with less precise tools, may underestimate what is possible for patients who are diagnosed early, treated with emerging therapies, and supported with evidence-based lifestyle interventions. The 2025 BMJ study provides the best current benchmark, but it is a snapshot of where things stand, not a ceiling on where they can go.
Conclusion
A dementia diagnosis at age 70 carries an average survival of roughly 7 to 10 years, with women typically living longer than men and Alzheimer’s disease offering a somewhat better prognosis than vascular or Lewy body dementia. The 2025 BMJ study, covering more than 5.5 million patients, confirms that while 90 percent of people survive the first year, only about one in five reaches the 10-year mark. These numbers are shaped by the type of dementia, the person’s sex, their overall health, and the stage at which they are diagnosed. For families, the most useful response to these statistics is not to fixate on a single number but to plan across the range.
Secure legal and financial arrangements early. Have honest conversations about care preferences while your loved one can still participate. Build a support network that can adapt as needs change. The years ahead after a diagnosis at 70 can still hold meaning, connection, and quality of life, particularly in the early and middle stages, but only if families use the time they have wisely rather than waiting for a crisis to force their hand.
Frequently Asked Questions
Is 7-10 years a guarantee for someone diagnosed with dementia at 70?
No. That range represents a statistical average across large populations. Individual survival can be as short as 2-3 years or as long as 15 or more, depending on the type of dementia, overall health, and rate of progression. The 2025 BMJ study found that only 21 percent of dementia patients survived to 10 years after diagnosis.
Does the type of dementia matter for life expectancy?
Significantly. Alzheimer’s disease has the longest average survival at 8-12 years, while vascular dementia averages about 4 years. Lewy body dementia falls in between at 5-7 years. The BMJ review found Alzheimer’s patients lived approximately 1.4 years longer than those with other dementia types.
Why do women live longer than men after a dementia diagnosis?
Women live approximately 20 percent longer than men after diagnosis, according to the 2025 BMJ study. The exact reasons are not fully understood but likely involve a combination of biological factors, hormonal differences, and the same underlying mechanisms that give women longer life expectancy in the general population.
Can lifestyle changes after diagnosis extend survival?
While no lifestyle change can reverse dementia, maintaining physical activity, social engagement, proper nutrition, and management of other health conditions such as diabetes and heart disease can influence the rate of progression and overall quality of life. These factors appear in the research as modifiers of survival outcomes.
At what point do most people with dementia need full-time care?
This varies widely, but many people transition from independent or lightly supported living to full-time care 3 to 5 years after diagnosis. The timeline depends on the dementia type, rate of progression, and the availability of family caregivers. Planning for this transition early gives families more options.
How does a dementia diagnosis at 70 compare to one at 80?
A person diagnosed at 70 will lose more years of life expectancy in absolute terms, roughly 7-10 years compared to their peers, while someone diagnosed at 80 loses about 3-4 years. However, the person diagnosed at 70 will typically live longer in total years after diagnosis because they are starting from a younger, generally healthier baseline.