The average lifespan after a dementia diagnosis at age 50 is approximately 7 to 10 years, with many individuals living considerably longer depending on the type of dementia, overall health, and other individual factors. A 2025 study published in the Journal of Neurology, Neurosurgery & Psychiatry found an average survival of nearly 9 years for early-onset dementia patients overall, while the NeedYD (Needs in Young-Onset Dementia) study reported a mean survival of roughly 10 years from formal diagnosis. Some people diagnosed at 50 live as long as 20 years, particularly when the disease is caught relatively early and the person maintains a healthy lifestyle. Johns Hopkins research placing median survival at nearly 9 years for a diagnosis at 65 suggests that someone diagnosed at 50 would fall at the higher end of these ranges, likely 10 or more years. But those numbers, while grounding, only tell part of the story.
A 50-year-old receiving a dementia diagnosis faces a fundamentally different reality than someone diagnosed at 75 or 85. They are likely still working, raising children, paying a mortgage, and planning decades of future life. The diagnosis doesn’t just shorten a timeline — it reshapes it entirely. People with young-onset dementia lose an estimated 10 to 15 years of life expectancy compared to peers without the condition, and mortality rates run 5 to 8 times higher than the general population of the same age. This article breaks down what survival statistics actually mean for someone diagnosed at 50, how different dementia subtypes affect the outlook, why gender and disease severity matter, what the research says about the pace of cognitive decline in younger patients, and what practical steps can influence quality of life in the years that follow a diagnosis.
Table of Contents
- How Long Can Someone Live After a Dementia Diagnosis at Age 50?
- How Much Does a Dementia Diagnosis at 50 Reduce Life Expectancy?
- Why Dementia Subtype Is One of the Strongest Predictors of Survival
- What Factors Can Influence Survival After an Early Dementia Diagnosis?
- The Paradox of Faster Cognitive Decline in Younger Dementia Patients
- Global Trends in Young-Onset Dementia Prevalence
- What the Future May Hold for Survival After Young-Onset Dementia
- Conclusion
- Frequently Asked Questions
How Long Can Someone Live After a Dementia Diagnosis at Age 50?
Survival after a dementia diagnosis at 50 varies widely, and the range itself is important to understand. The NeedYD study found mean survival of approximately 17.4 years from the onset of symptoms but roughly 10 years from the point of formal diagnosis. That gap matters. Dementia in younger people is frequently misdiagnosed or overlooked for years — attributed to stress, depression, or burnout — meaning the disease may have been progressing for seven or more years before anyone names it. A 50-year-old who receives a diagnosis may have been experiencing subtle symptoms since their early to mid-40s. Median survival also differs by subtype. Alzheimer’s disease, the most common form even in younger patients, carries a median survival of about 11.3 years from age of onset.
Frontotemporal dementia follows closely at 10.6 years, while vascular dementia comes in at approximately 12.3 years. The outlier is the combination of frontotemporal dementia with motor neurone disease, where survival drops to roughly 2 years. Consider two people both diagnosed at 50: one with early-onset Alzheimer’s might live into their early 60s, while another with frontotemporal dementia and motor neurone disease may not reach 53. The subtype is not a footnote — it is a defining variable. Johns Hopkins research reinforces the general principle that younger age at diagnosis correlates with longer survival time. Their data showed median survival of nearly 9 years for a diagnosis at 65 and about 3 years for a diagnosis at 90. Extrapolating from this curve, a diagnosis at 50 places an individual at the upper end, where survival of 10 years or more is a reasonable expectation rather than an exception. Some individuals, particularly those with strong physical health and robust support systems, have lived 15 to 20 years after diagnosis.

How Much Does a Dementia Diagnosis at 50 Reduce Life Expectancy?
The raw survival numbers don’t fully capture the impact unless you compare them against what would have been expected without the diagnosis. A healthy 50-year-old in the general population can reasonably expect to live into their late 70s or 80s. A dementia diagnosis dramatically compresses that horizon. Research shows that remaining life expectancy is reduced by 51 percent for males and 59 percent for females compared to age-matched peers without dementia. A 2019 study found that people with early-onset Alzheimer’s live 59 percent shorter lives than the general population — not 59 percent shorter than average dementia patients, but 59 percent shorter than healthy people their age. To put that in concrete terms: if a 50-year-old man without dementia would be expected to live to 80, a 51 percent reduction in remaining life expectancy would place his projected lifespan around 65. For a 50-year-old woman who might otherwise live to 83, a 59 percent reduction points to roughly 63 or 64.
These are statistical averages, not individual sentences, but they illustrate how severe the reduction is. Separate research found that a dementia diagnosis at age 65 reduced life expectancy by about 13 years; at age 50, the absolute reduction may be even larger because the person had more years to lose. However, these figures come with a critical caveat. They are population-level statistics drawn from cohorts that include people diagnosed at various stages of severity, with different subtypes, and with varying levels of comorbidity. A 50-year-old diagnosed in the early stages of Alzheimer’s disease, with no other major health conditions, who has access to strong medical care and family support, may well outperform these averages. Conversely, someone diagnosed at the same age but with significant vascular disease, diabetes, or late-stage symptoms may fall below them. The averages describe a landscape, not a destination.
Why Dementia Subtype Is One of the Strongest Predictors of Survival
Not all dementias behave the same way, and the specific diagnosis a 50-year-old receives matters enormously. Alzheimer’s disease patients survive approximately 1.4 years longer on average than those with other forms of dementia, including vascular, frontotemporal, and Lewy body variants. This may seem like a modest difference in isolation, but across a population it is statistically significant, and for an individual weighing their future, an extra year and a half is not trivial. Frontotemporal dementia deserves particular attention in the context of a diagnosis at 50 because it disproportionately affects younger people. While Alzheimer’s accounts for most dementia cases across all ages, frontotemporal dementia makes up a much larger share of early-onset cases. Its behavioral variant can initially look like a psychiatric condition — personality changes, impulsivity, social disinhibition — which often delays accurate diagnosis.
The language variants erode communication in ways that differ sharply from the memory-dominant pattern of Alzheimer’s. And when frontotemporal dementia co-occurs with motor neurone disease, the prognosis collapses to around 2 years, making it the most aggressive combination in the young-onset category. Take the example of a 50-year-old diagnosed with behavioral variant frontotemporal dementia versus one diagnosed with early-onset Alzheimer’s. The frontotemporal patient might retain memory relatively well in the early years but struggle profoundly with judgment, empathy, and social behavior — sometimes leading to job loss, legal trouble, or family breakdown before anyone suspects dementia. The Alzheimer’s patient might maintain social graces longer but lose the ability to remember recent conversations or navigate familiar routes. Both are devastating, but the trajectory, the care needs, and the survival timeline differ in ways that demand subtype-specific planning rather than a one-size approach.

What Factors Can Influence Survival After an Early Dementia Diagnosis?
Several variables interact to shape how long and how well someone lives after a dementia diagnosis at 50, and understanding them helps families plan rather than simply wait. Gender is one of the clearest: women with Alzheimer’s disease live on average 20 percent longer than men after diagnosis. The reasons are not fully understood, but likely involve a combination of biological factors, differences in health-seeking behavior, and the social support structures that tend to differ between men and women. A man and a woman both diagnosed with Alzheimer’s at 50 may face meaningfully different timelines. Disease severity at the time of diagnosis is another powerful predictor. People who already exhibit wandering, frequent falls, or incontinence at diagnosis tend to have shorter survival than those caught at an earlier functional stage.
This creates a practical tradeoff: pursuing an early diagnosis can feel terrifying, and many families delay seeking evaluation because they are afraid of the answer. But earlier diagnosis generally means diagnosis at a less severe stage, which correlates with more time — and more time at higher levels of independence and quality of life. The years gained by early detection are not just years added to the end; they are years preserved at the front, when the person can still participate in decisions about their own care, finances, and legacy. Comorbidities — other health conditions like heart disease, diabetes, hypertension, or chronic lung disease — also strongly influence survival. A 50-year-old with dementia and no other major health issues is in a fundamentally different position than one with dementia layered on top of poorly controlled diabetes and cardiovascular disease. Managing those coexisting conditions aggressively does not slow the dementia itself, but it can prevent the secondary medical crises that often shorten life in dementia patients.
The Paradox of Faster Cognitive Decline in Younger Dementia Patients
One of the more counterintuitive findings in dementia research is that while younger patients survive longer in absolute terms, they often experience faster cognitive decline. Young people with Alzheimer’s lose cognitive function more rapidly than older Alzheimer’s patients, even though they live more years overall. This means the disease is not simply a slower version of what an 80-year-old would experience — it is often more aggressive in its progression through cognitive domains, even as the younger body sustains life longer. This has real consequences for care planning. Families of a 50-year-old with dementia might assume that because the prognosis is “better” than for an older patient — more years of survival — the disease will be gentler along the way. It may not be.
The period of moderate to severe impairment can stretch over many years, creating sustained demands on caregivers that differ from the pattern seen in late-onset cases where the total caregiving timeline is compressed. Financial planning, caregiver rotation, and long-term residential care decisions all need to account for a potentially prolonged period of high-dependency care. There is also an emotional dimension that statistics cannot capture. A 50-year-old declining rapidly is often still physically robust, which creates a dissonance between physical capability and cognitive capacity. They may be strong enough to wander miles from home but unable to remember where they live. They may look healthy to acquaintances who then question why they cannot work. Caregivers of younger dementia patients consistently report higher levels of stress, isolation, and grief than caregivers of older patients, in part because the social infrastructure of aging — retirement communities, elder care systems, Medicare — does not fit a person in their 50s.

Global Trends in Young-Onset Dementia Prevalence
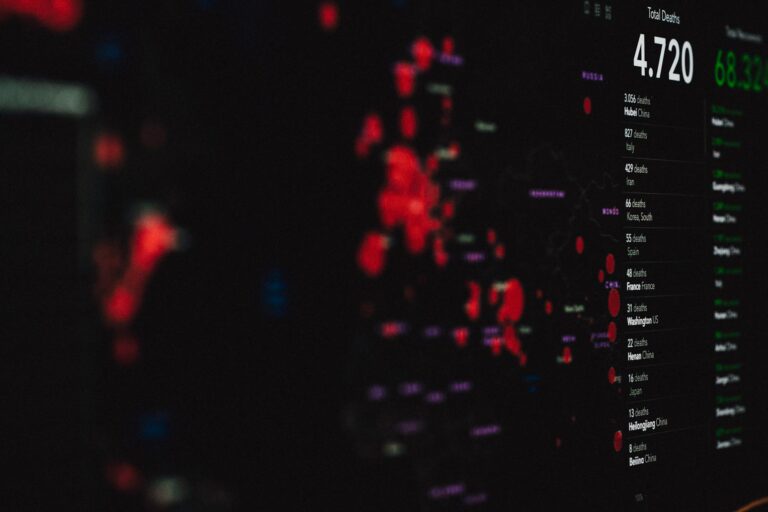
The number of people facing a dementia diagnosis at 50 or younger is not static. Global age-standardized prevalence of dementia in people under 65 rose from 93.39 per 100,000 in 1990 to 96.09 per 100,000 in 2021, according to a 2025 study published in Translational Psychiatry.
That increase is modest in percentage terms but represents a meaningful number of additional people and families affected worldwide, particularly as global populations grow and life expectancy in middle-income countries improves. This trend makes the survival and quality-of-life questions discussed throughout this article increasingly urgent. If more people are developing dementia before age 65, then the health systems, workplace policies, disability frameworks, and family support structures in most countries will face growing pressure from a population of patients that doesn’t fit neatly into existing models designed primarily for elderly care.
What the Future May Hold for Survival After Young-Onset Dementia
Research into disease-modifying treatments has accelerated in recent years, with several anti-amyloid therapies now approved or in late-stage trials for Alzheimer’s disease. While their effects to date have been modest — slowing decline rather than stopping or reversing it — they represent a shift from purely symptomatic management toward addressing underlying disease mechanisms. For a 50-year-old diagnosed today, even incremental advances over the next decade could meaningfully extend both survival and the period of preserved function.
Equally important are improvements in early detection. Blood-based biomarker tests for Alzheimer’s are becoming more accurate and accessible, which could shift the average point of diagnosis earlier in the disease course. If the NeedYD study’s finding holds — that symptoms precede formal diagnosis by roughly 7 years — then closing that gap would not necessarily change how long the disease lasts, but it would give patients and families more years of awareness and preparation. For someone at 50, those extra years of planning time can mean the difference between financial ruin and stability, between crisis-driven caregiving and structured support.
Conclusion
A dementia diagnosis at age 50 carries an average survival of roughly 7 to 10 years from formal diagnosis, with considerable variation based on dementia subtype, gender, disease severity, comorbidities, and individual factors. Alzheimer’s disease tends to allow the longest survival among common subtypes, and younger age at diagnosis generally correlates with more years of life — though often accompanied by faster cognitive decline. The reduction in life expectancy is severe, cutting remaining years by roughly half compared to peers without dementia, and mortality rates run 5 to 8 times higher than the general population of the same age. The numbers are sobering, but they are not the whole story.
Some individuals live 15 to 20 years after diagnosis. Early detection, aggressive management of other health conditions, strong caregiving support, and emerging treatments can all influence the trajectory. For anyone facing this diagnosis or supporting someone who is, the most productive response is not to fixate on averages but to plan for a range of outcomes — securing financial and legal protections early, building a care team, staying physically active, and making the most of the years of highest function. The statistics describe probabilities; they do not dictate an individual life.
Frequently Asked Questions
Is early-onset dementia the same as Alzheimer’s disease?
No. Early-onset dementia refers to any dementia diagnosed before age 65, and it can include Alzheimer’s disease, frontotemporal dementia, vascular dementia, Lewy body dementia, and rarer forms. Alzheimer’s is the most common subtype, but frontotemporal dementia accounts for a larger share of young-onset cases than it does in the elderly population.
Can someone diagnosed with dementia at 50 still work?
In many cases, yes — at least for a period after diagnosis. How long depends on the type of dementia, the nature of the work, and how quickly symptoms progress. Some people continue working in modified roles for a year or more after diagnosis, while others find that cognitive demands outpace their abilities relatively quickly. Early legal and financial planning is essential.
Does dementia at 50 always run in families?
Not always. While genetic factors play a larger role in early-onset cases than in late-onset dementia, many people diagnosed at 50 have no known family history. Certain genetic mutations, particularly in the APP, PSEN1, and PSEN2 genes, cause familial Alzheimer’s that can appear in the 40s and 50s, but these account for a small fraction of all cases.
Why do women with Alzheimer’s live longer than men after diagnosis?
The exact reasons are not fully established. Research shows women with Alzheimer’s live on average 20 percent longer than men after diagnosis. Contributing factors likely include biological differences in how the disease progresses, differences in overall health and comorbidity profiles, and potentially differences in caregiving patterns and social support.
What is the most aggressive form of young-onset dementia?
Frontotemporal dementia combined with motor neurone disease carries the shortest survival, approximately 2 years from onset. This combination is relatively rare but devastating, as it affects both cognition and motor function simultaneously.
Does a healthy lifestyle slow dementia progression?
There is no proven way to stop dementia progression once it has started. However, physical exercise, cardiovascular health management, cognitive engagement, and social connection are associated with better overall outcomes and may help preserve function longer. Managing comorbidities like diabetes and hypertension is particularly important, as these conditions can accelerate decline independently.