Swallowing difficulties in late-stage dementia follow a rough but recognizable timeline. In Alzheimer’s disease, subtle oral-phase impairments begin early, pharyngeal problems emerge in the moderate stage, and full swallowing apraxia — the loss of the motor ability to swallow — sets in during the severe stage. By the time dementia is moderate to severe, between 84 and 93 percent of patients experience some form of dysphagia. For families watching a parent or spouse struggle with meals, understanding this progression is not academic. It is the difference between panic and preparation. Consider a woman whose mother was diagnosed with Alzheimer’s at 72. For the first few years, the only signs were occasional coughing at dinner and a tendency to pocket food in her cheeks.
By year five, thickened liquids became necessary. By year seven, she was aspirating silently — inhaling small amounts of food and saliva without any visible cough — and developed pneumonia twice in six months. That trajectory, while painful, is typical. This article maps out the timeline of swallowing decline, explains why aspiration pneumonia is the leading cause of death in end-stage Alzheimer’s, examines what the evidence actually says about feeding tubes, and outlines the comfort-focused approaches that current medical guidelines recommend. The timeline also varies by dementia type. In frontotemporal dementia, dysphagia tends to develop only in the late stages, while Alzheimer’s disease produces subtle signs much earlier. Knowing which type of dementia you are dealing with matters for anticipating when swallowing will become a crisis rather than an inconvenience.
Table of Contents
- When Do Swallowing Difficulties Start in Dementia, and How Fast Do They Progress?
- Why Aspiration Pneumonia Is the Leading Cause of Death in Late-Stage Dementia
- The Natural Decline of Eating and Drinking at the End of Life
- Feeding Tubes in Advanced Dementia — What the Evidence Actually Shows
- Silent Aspiration and the Limits of Caregiver Detection
- Comfort-Focused Approaches That Current Guidelines Recommend
- Planning Ahead — Why the Conversation Needs to Happen Before the Crisis
- Conclusion
- Frequently Asked Questions
When Do Swallowing Difficulties Start in Dementia, and How Fast Do They Progress?
The progression of dysphagia in dementia is not a cliff but a slope. In Alzheimer’s disease, the earliest signs are oral-phase impairments — difficulty chewing, holding food in the mouth too long, or forgetting the sequence of chewing and swallowing. These problems are often subclinical, meaning they do not cause obvious distress but can be detected on a clinical swallowing evaluation. As the disease moves into moderate stages, pharyngeal symptoms appear: food gets stuck in the throat, coughing during meals becomes frequent, and the swallow reflex weakens. In severe Alzheimer’s, swallowing apraxia takes hold — the brain can no longer coordinate the muscles needed to swallow at all. Among institutionalized dementia patients, roughly 45 percent have clinically significant dysphagia.
That number climbs dramatically in the final stages. In nursing home residents with advanced dementia, researchers have documented an approximately 300-day lag between the onset of recognizable eating problems and the development of life-threatening pneumonia. Three hundred days is not a lot of runway, but it is enough time for families to have critical conversations about goals of care, advance directives, and what comfort looks like in practice. The comparison between Alzheimer’s and frontotemporal dementia is worth noting again because it catches families off guard. A person with behavioral-variant FTD may eat voraciously and without any swallowing trouble for years, then decline rapidly once dysphagia finally appears. A person with Alzheimer’s, by contrast, may show small signs for a long time before the situation becomes dangerous. Neither pattern is better or worse — they simply require different vigilance at different points.

Why Aspiration Pneumonia Is the Leading Cause of Death in Late-Stage Dementia
Aspiration pneumonia is the most common cause of death in end-stage Alzheimer’s disease, and the mechanism is straightforward. When the swallow reflex fails, food, liquid, and oral bacteria slide into the lungs instead of the stomach. The lungs become infected. In a person whose immune system is already compromised by advanced illness and immobility, that infection is often fatal. Dementia patients with dysphagia face twice the risk of dying from aspiration pneumonia compared to those who do not aspirate. Among people with advanced dementia who develop aspiration pneumonia, 46.7 percent die within six months. That statistic is sobering, but it also clarifies something families need to hear: aspiration pneumonia in this context is not a treatable infection that antibiotics will cure and the person will bounce back from.
It can be treated, and sometimes the person does recover temporarily, but recurrence is the norm because the underlying swallowing dysfunction does not improve. Each episode of pneumonia tends to leave the person weaker and more vulnerable to the next one. Silent aspiration deserves special attention because it is so commonly missed. When a person aspirates silently, food or liquid enters the airway without triggering a cough. There is no choking episode, no dramatic moment at the dinner table. The caregiver may have no idea anything went wrong until a fever develops days later. This is one reason why families sometimes feel blindsided by a pneumonia diagnosis — they thought mealtimes were going fine. If a person with advanced dementia develops recurrent fevers or unexplained respiratory symptoms, silent aspiration should be high on the list of suspected causes, even if meals appear uneventful.
The Natural Decline of Eating and Drinking at the End of Life
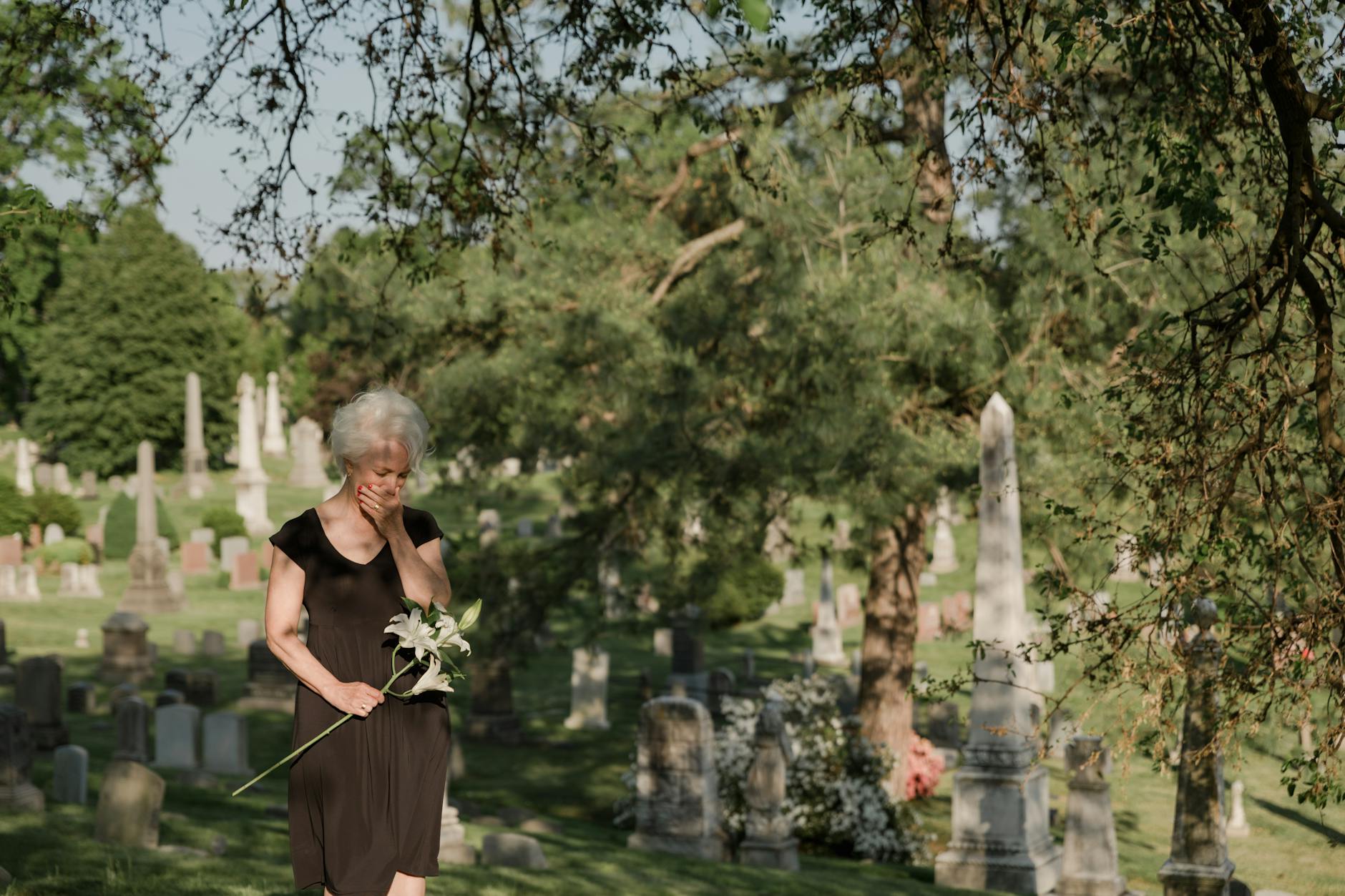
As dementia reaches its final stages, food and fluid intake tends to decrease slowly over time. This gradual decline is not a failure of caregiving. It is the body winding down. The Alzheimer’s Society UK notes that a significant decline in intake typically occurs one to three weeks before death. For families who have spent months or years focused on getting their loved one to eat enough, this shift can feel agonizing. The instinct to feed is one of the deepest human impulses, and watching someone refuse food triggers a grief response that is hard to override with medical reasoning. If a person with dementia stops eating and drinking entirely, death typically occurs within a few days to approximately ten days. That range depends on factors like the person’s overall hydration status, body composition, and whether small amounts of fluid are still being absorbed through mouth care. It is important to understand that this timeline, while distressing to read on a page, often unfolds with less suffering than families fear.
Current evidence supports that the body adjusts during the dying process so that patients do not experience hunger or thirst as intake naturally declines. The metabolic changes of active dying produce a kind of natural analgesia. A daughter caring for her father at home described this period as the hardest and the most peaceful at the same time. He stopped asking for food. He stopped opening his mouth when she brought a spoon close. She kept his lips moist with a damp sponge and sat with him. He died six days later, without any sign of distress. That experience, while individual, reflects what palliative care clinicians observe regularly. The suffering during this phase tends to belong more to the family than to the patient.

Feeding Tubes in Advanced Dementia — What the Evidence Actually Shows
Few decisions in dementia care carry as much emotional weight as whether to place a feeding tube. The instinct is understandable: if someone cannot eat, a tube that delivers nutrition directly to the stomach seems like an obvious solution. But the evidence is clear and has been consistent for more than two decades. Feeding tubes in advanced dementia have not been shown to prevent aspiration pneumonia, heal or prevent pressure sores, improve functional status, provide comfort, or extend life. The numbers are grim. In-hospital mortality when a feeding tube is placed in this population runs between 15 and 25 percent. One-year mortality after placement is 60 percent.
A meta-analysis found that PEG tube feeding in advanced dementia is actually associated with a significantly higher risk of pneumonia and pressure sores — the very outcomes families hope the tube will prevent. The tube does not stop aspiration because patients continue to aspirate their own saliva and gastric contents, which reflux upward from the stomach. Meanwhile, the tube itself introduces new complications: infection at the insertion site, agitation that leads to physical restraints, and the loss of the social and sensory experience of being fed by hand. Careful hand feeding, by comparison, showed no difference in one-year survival compared to nasogastric tube feeding — 37 percent versus 36 percent — but with reduced pneumonia risk. Hand feeding is slower, more labor-intensive, and requires patience and skill. But it preserves human contact, allows the person to taste food, and avoids the complications of a surgical procedure in someone who is actively dying. The tradeoff is not between nutrition and no nutrition. It is between a medical intervention that does not work and a human one that does roughly the same thing with fewer harms.
Silent Aspiration and the Limits of Caregiver Detection
One of the most dangerous aspects of swallowing decline in dementia is how invisible it can be. Silent aspiration — inhaling food, liquid, or saliva into the lungs without coughing — is common in advanced dementia and often goes completely undetected by caregivers. A person can silently aspirate at every meal for weeks before the resulting lung infection becomes apparent. By then, the damage is done. This is a genuine limitation of home-based and even institutional caregiving. No amount of vigilance at the dinner table can catch what the body does not signal. A videofluoroscopic swallowing study (a real-time X-ray of swallowing) can detect silent aspiration, but it requires a clinical setting, cooperation from the patient, and the results offer a snapshot rather than ongoing monitoring.
For many people with advanced dementia, the test itself is impractical. Families should understand that even with the best care, aspiration events will happen. The goal shifts from prevention to harm reduction: smaller meals, modified textures, upright positioning during and after eating, and excellent oral hygiene to reduce the bacterial load that enters the lungs when aspiration occurs. A warning for families navigating this: do not let guilt over an aspiration pneumonia diagnosis consume you. It is not caused by a caregiver feeding someone incorrectly. It is caused by a degenerative brain disease that has destroyed the neural pathways controlling swallowing. The best caregivers in the world cannot prevent what the brain can no longer coordinate.
Comfort-Focused Approaches That Current Guidelines Recommend
The British Geriatrics Society recommends comfort-focused approaches in advanced dementia, including careful hand feeding, modified food textures, and good oral hygiene — not feeding tubes. These are not passive measures. Proper hand feeding requires training: reading the person’s cues, offering small amounts, waiting for each swallow before offering more, and stopping when the person shows signs of fatigue or refusal. Modified textures — pureed foods, thickened liquids — reduce but do not eliminate aspiration risk.
Good oral hygiene is arguably the most underappreciated intervention. A clean mouth means fewer bacteria available to cause pneumonia when aspiration does occur. Brushing teeth and gums, using mouth swabs, and treating oral infections are concrete steps that directly reduce the deadliest complication of dysphagia. For a caregiver looking for something actionable in a situation that feels helpless, mouth care is it.
Planning Ahead — Why the Conversation Needs to Happen Before the Crisis
The 300-day window between the onset of eating problems and life-threatening pneumonia is not just a clinical data point. It is a planning window. Families who use that time to discuss goals of care, complete or update advance directives, and consult with palliative care teams are better prepared — not for a good outcome, because there is no good outcome in end-stage dementia, but for a less chaotic one.
The hardest part of these conversations is their finality. Deciding against a feeding tube, agreeing to comfort-focused care, signing a do-not-hospitalize order — these feel like giving up. They are not. They are a recognition that the disease has reached a stage where medical interventions cause more suffering than they relieve, and that the most loving thing a family can do is ensure their person is comfortable, clean, and not alone.
Conclusion
Swallowing difficulties in dementia follow a timeline that, while variable, is broadly predictable. Early oral-phase problems give way to pharyngeal dysfunction, then to swallowing apraxia, and ultimately to aspiration pneumonia — the leading cause of death in end-stage Alzheimer’s. Between 84 and 93 percent of patients with moderate-to-severe Alzheimer’s experience dysphagia, and nearly half of those who develop aspiration pneumonia die within six months.
Feeding tubes do not change these outcomes. Careful hand feeding, modified textures, and meticulous oral hygiene are what the evidence supports. For families in the middle of this, the most important steps are practical: talk to a speech-language pathologist about swallowing safety strategies, discuss goals of care with the medical team before a crisis forces the conversation, and understand that the natural decline in eating and drinking at the end of life is not starvation — it is the body’s way of shutting down, and the person is likely not suffering from it the way you fear. Your presence, your voice, and the comfort you provide matter more than any calorie count.
Frequently Asked Questions
How long can a person with dementia live after they stop eating and drinking?
If a person with dementia stops eating and drinking entirely, death typically occurs within a few days to approximately 10 days. The exact timeline depends on hydration status, body composition, and overall condition. Current evidence suggests the person does not feel hunger or thirst during this process.
Do feeding tubes help people with advanced dementia live longer?
No. Research consistently shows that feeding tubes in advanced dementia do not extend life, prevent aspiration pneumonia, heal pressure sores, or improve comfort. One-year mortality after feeding tube placement is approximately 60 percent. Careful hand feeding produces comparable survival rates with fewer complications.
What is silent aspiration, and why is it dangerous?
Silent aspiration occurs when food, liquid, or saliva enters the lungs without triggering a cough. It is common in advanced dementia and often goes undetected by caregivers. Because there is no visible choking, infections can develop in the lungs before anyone realizes aspiration has occurred.
Does dysphagia develop at the same time in all types of dementia?
No. In Alzheimer’s disease, subtle swallowing problems begin in the early stages and worsen progressively. In frontotemporal dementia, dysphagia tends to appear only in the late stages. The type of dementia affects when families should begin watching for swallowing difficulties.
What can caregivers do to reduce aspiration risk?
Key strategies include keeping the person upright during and for 30 minutes after meals, offering small bites and sips, using modified food textures such as pureed foods and thickened liquids, maintaining good oral hygiene to reduce bacteria in the mouth, and stopping feeding when the person shows signs of fatigue or refusal.
Is it cruel to stop offering food to someone with end-stage dementia?
Following the person’s cues — including the cue of refusing food — is not cruel. The British Geriatrics Society and other medical organizations recommend comfort-focused care that respects the person’s natural decline. Evidence indicates that patients in this stage do not experience hunger or thirst as their body adjusts to the dying process.





