The best cushion for a dementia patient after hospital discharge is a high-specification reactive foam or gel-hybrid pressure redistributing cushion, selected based on an individual risk assessment rather than a one-size-fits-all recommendation. For someone at moderate risk, a product like the Cushion Lab Pressure Relief Seat Cushion (around $60–70) or the Purple Seat Cushion ($60–80) offers meaningful pressure redistribution at a reasonable price point. For patients at very high risk of pressure ulcers, a medical-grade alternating pressure system such as the Viola II Alternating Pressure Relief Cushion System may be necessary. The critical point is that cushion selection should be guided by clinical assessment, ideally by an occupational therapist or tissue viability specialist, not by browsing online reviews alone. This matters more than most families realize. Research published in BMC Geriatrics found that 67% of geriatric patients with pressure ulcers had dementia, compared to only 23% of those without pressure ulcers.
The connection between dementia and skin breakdown is not incidental. It is driven by immobility, incontinence, poor nutrition, and the loss of the instinct to shift weight while seated. A person with mid-stage Alzheimer’s who has just been discharged from the hospital after a hip repair, for example, may sit in a recliner for hours without repositioning, rapidly developing dangerous pressure points over the sacrum and ischial tuberosities. The right cushion is not a luxury. It is a basic safety measure. This article covers why dementia patients face such elevated pressure ulcer risk after hospital discharge, what the clinical guidelines actually recommend, how to compare cushion types and materials, what to look for in covers and accessories, how to avoid common mistakes like ring cushions and “bottoming out,” and what new international guidelines are saying about seated pressure care heading into 2026.
Table of Contents
- Why Do Dementia Patients Need Specialized Cushions After Hospital Discharge?
- What Do Clinical Guidelines Recommend for Pressure Relief Cushions?
- How Do Different Cushion Types Compare for Dementia Care?
- What Features Should You Look for in a Cushion Cover and Construction?
- Common Mistakes That Increase Pressure Ulcer Risk After Discharge
- How NHS and Insurance Aftercare Can Help With Cushion Provision
- What New International Guidelines Mean for Seated Pressure Care
- Conclusion
Why Do Dementia Patients Need Specialized Cushions After Hospital Discharge?
The period immediately following hospital discharge is one of the most dangerous windows for a person living with dementia. All-cause 30-day readmission rates for people with dementia range from 7% to 35%, significantly higher than for those without cognitive impairment, and roughly 20–40% of these readmissions may be preventable. dementia patients face twice the risk of hospital readmission compared to cognitively intact older adults, and a substantial portion of those readmissions involve complications like pressure ulcers that could have been mitigated with proper equipment and care planning at home. The statistics around pressure ulcers in this population are stark. A study published in the Journal of the American Medical Directors Association found that almost 40% of advanced dementia patients developed pressure ulcers before death. Even more striking, median survival for advanced dementia patients with pressure ulcers was just 96 days, compared to 863 days for those without — a nearly ninefold difference.
While a pressure ulcer does not directly cause death in most cases, it serves as both a marker of deteriorating overall condition and a compounding factor that accelerates decline through pain, infection, reduced mobility, and increased hospitalization. Consider the common scenario: a 78-year-old woman with moderate vascular dementia is discharged home after treatment for a urinary tract infection. She is weaker than before admission, less mobile, and more confused. She spends most of her day in an armchair or wheelchair. If that chair has only a standard foam cushion — or worse, no cushion at all — pressure begins to concentrate over bony prominences within minutes. Dementia patients are twice as likely to experience adverse events in hospital, including pressure injuries, and face a fivefold increase in mortality rates. The transition home, where professional monitoring drops away, is when the risk intensifies rather than resolving.

What Do Clinical Guidelines Recommend for Pressure Relief Cushions?
The most widely referenced clinical standard for pressure ulcer prevention in the UK is NICE Clinical Guideline CG179, which recommends high-specification reactive foam or equivalent pressure redistributing cushions for adults who use a wheelchair or sit for prolonged periods. This is not a suggestion to grab any foam pad from a department store. “High-specification” refers to cushions engineered with specific densities, layered materials, or active pressure redistribution technology that meaningfully reduces interface pressure at the sitting surface. The guideline applies to anyone at elevated risk, but it is especially relevant for dementia patients, who frequently lack the ability to recognize discomfort and shift their weight independently. Internationally, there is growing recognition that seated pressure care has been under-addressed. The European Pressure Ulcer Advisory Panel (EPUAP), the National Pressure Injury Advisory Panel (NPIAP), and the Pan Pacific Pressure Injury Alliance are developing a new seating-specific chapter as part of their international pressure ulcer clinical practice guideline, with stakeholder feedback open until February 1, 2026.
In December 2025, a dedicated document titled “Preventing pressure injuries in Seated Individuals” was published, reflecting the acknowledgment that existing guidelines have focused heavily on bed-based pressure relief while giving inadequate attention to the hours patients spend sitting. However, guidelines alone do not solve the problem if families are not connected with the right professionals. Cushion selection should be individualized through assessment by an occupational therapist or tissue viability specialist, according to clinical best practice recommendations. A cushion that works well for one patient may be entirely wrong for another, depending on body weight, existing skin damage, continence status, posture, and the specific seating system being used. If a patient is discharged on a Friday afternoon with no therapy follow-up scheduled for two weeks, the family is essentially on their own during the highest-risk period. In the UK, NHS intermediate care provides six weeks of free aftercare after hospital discharge, which can include equipment provision, but families often need to proactively request this rather than waiting to be offered it.
How Do Different Cushion Types Compare for Dementia Care?
The consumer and medical cushion market breaks down into several broad categories, each with distinct tradeoffs for dementia patients. Memory foam cushions, such as the ComfiLife Gel Enhanced Seat Cushion (approximately $35–45), use body heat to conform to the user’s shape, distributing weight across a larger surface area and reducing peak pressure points. The ComfiLife model adds a cooling gel layer and a coccyx cutout, which can relieve tailbone pressure. These are the most affordable option and work well for patients at low to moderate risk, but they do have a limitation: memory foam retains heat, and for a dementia patient who is incontinent and sits for extended periods, heat buildup can increase moisture at the skin surface, raising the risk of maceration and skin breakdown. Gel-based and hybrid cushions take a different approach. The Purple Seat Cushion ($60–80) uses a hyper-elastic polymer grid that flexes under pressure, distributing weight more evenly than traditional foam without the heat retention problem.
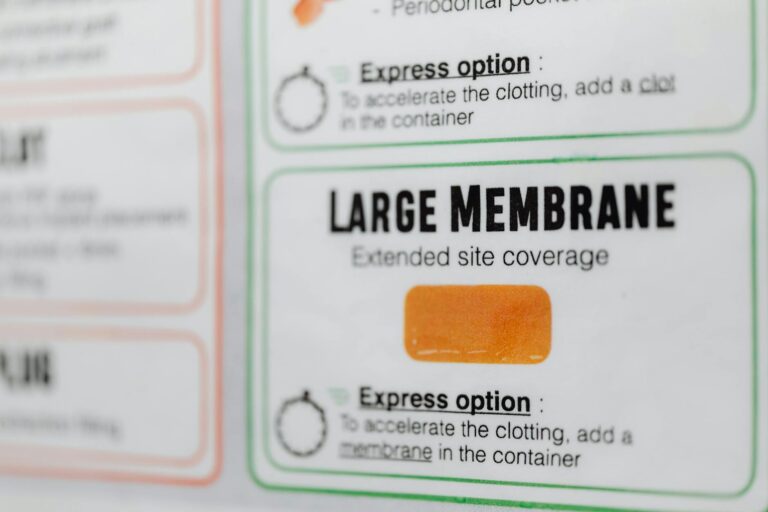
The Cushion Lab Pressure Relief Seat Cushion ($60–70) uses a patented multi-region design recommended by physical therapists, with firmer zones at the edges for stability and softer zones under pressure-sensitive areas. For a dementia patient who tends to slide forward in a chair — a common issue related to reduced proprioception and postural control — the Cushion Lab’s zoned design may offer an advantage over a uniform-density cushion. At the higher end, the Tempur-Pedic Seat Cushion (around $89) provides firm, premium material support, while the Viola II Alternating Pressure Relief Cushion System represents a different category entirely. The Viola II is a medical-grade alternating pressure system designed for patients at very high risk of pressure ulcers, using air cells that cyclically inflate and deflate to actively shift pressure points. This is the type of cushion a tissue viability nurse might prescribe for a patient with Stage 2 or higher pressure damage, or for someone who cannot be repositioned frequently. It is not available at retail stores, is significantly more expensive, and requires clinical setup, but for the right patient, it can be the difference between wound healing and wound deterioration.

What Features Should You Look for in a Cushion Cover and Construction?
The cushion itself is only part of the equation. For dementia patients, the cover and construction details matter enormously because of the high prevalence of incontinence in this population. Incontinence is one of the key risk factors for pressure ulcer development, alongside immobility, poor nutritional status, significantly lower hemoglobin and serum albumin levels, and impaired sensation. A cushion that absorbs urine becomes a breeding ground for bacteria and rapidly loses its pressure-redistributing properties as the foam or gel breaks down. Clinical best practice recommends incontinence-friendly covers with waterproof construction and waterfall flap zippers that prevent fluid from seeping into the cushion interior. The cover material should be breathable and vapor-permeable — fabrics like Dartex are commonly used in clinical settings because they block liquid penetration while allowing moisture vapor to escape, reducing the humidity trapped against the skin.
This is a meaningful tradeoff: fully sealed plastic covers are waterproof but trap heat and moisture, worsening the microclimate at the skin surface. Vapor-permeable covers cost more but are clinically superior for extended sitting. There is also the question of how the cushion integrates with the seating system. A pressure-relief cushion placed on a standard dining chair behaves very differently than the same cushion secured to a tilt-in-space recliner. Tilt-in-space seating combined with pressure-relieving cushions forms the basis of a comprehensive pressure care strategy, because tilting the seat redistributes weight across the back and thighs rather than concentrating it on the ischial tuberosities. If the family’s budget or space allows for only one investment, a tilt-in-space chair with a good cushion will generally outperform an excellent cushion on a flat, rigid chair.
Common Mistakes That Increase Pressure Ulcer Risk After Discharge
The single most widespread mistake families make is purchasing a doughnut-shaped or ring cushion, believing that the central cutout will relieve pressure on the tailbone. Doughnut-type ring cushions should be avoided entirely. Clinical evidence and the 2023 Wound Healing Society guidelines update confirm that ring cushions increase venous congestion and edema in the tissues surrounding the cutout by concentrating pressure in a smaller ring-shaped area. Rather than distributing weight more broadly, they create a tourniquet effect that reduces blood flow to the very tissues most vulnerable to breakdown. They are still widely sold online and even recommended in some outdated consumer articles, which makes this a persistent problem. The second common mistake is failing to check for “bottoming out.” Bottoming out occurs when a cushion compresses to the point that it no longer meaningfully redistributes pressure — the user can feel the hard surface beneath through the cushion. NICE guidelines specifically recommend that cushions be regularly assessed for this.
A simple test: place your hand, palm up, under the cushion beneath the patient’s ischial tuberosities (the bony prominences you sit on). If you can feel the bones pressing through the cushion against your hand with less than an inch of material providing resistance, the cushion has bottomed out and needs replacement. Foam cushions degrade faster than gel or air-based systems, and a cushion that was adequate three months ago may be providing almost no protection today. A third and less obvious mistake involves agitation and repositioning. Dementia patients in later stages may become agitated or restless, pulling at cushions, sliding out of position, or resisting repositioning attempts. Difficulty eating and swallowing, lack of proprioception, agitation, and social isolation in late-stage dementia all compound pressure ulcer risk. A cushion that is technically excellent but repeatedly displaced or bunched up under the patient provides no benefit. Securing systems, anti-slip bases, and cushion selection that accounts for the patient’s behavioral patterns are all important considerations that require professional assessment rather than guesswork.

How NHS and Insurance Aftercare Can Help With Cushion Provision
Many families do not realize that they may not need to purchase a pressure relief cushion out of pocket. In the UK, NHS intermediate care provides six weeks of free aftercare after hospital discharge, which can include provision of pressure-relieving equipment such as cushions, mattresses, and seating systems. This service is typically coordinated through occupational therapy and community nursing teams, but it often needs to be specifically requested during discharge planning. The Alzheimer’s Society recommends that families ask about equipment provision before leaving the hospital, rather than waiting until a problem develops at home.
In the United States, Medicare Part B may cover seat cushions classified as durable medical equipment when prescribed by a physician and deemed medically necessary, though coverage criteria are strict and typically require documented existing pressure ulcer risk or injury. Private insurance coverage varies widely. Regardless of the payment mechanism, the key action is the same: request a clinical assessment of the patient’s seating and pressure care needs before or immediately after discharge. A $60 cushion purchased proactively is far less costly — in every sense — than a hospital readmission for a Stage 3 pressure ulcer.
What New International Guidelines Mean for Seated Pressure Care
The development of a dedicated seating chapter in the international pressure ulcer clinical practice guideline represents a significant shift in how the clinical community views seated pressure injury prevention. Historically, the overwhelming focus has been on mattress selection and bed-based repositioning schedules, while the hours patients spend in wheelchairs, recliners, and standard chairs received comparatively little structured guidance. The December 2025 publication of “Preventing Pressure Injuries in Seated Individuals” by the EPUAP, NPIAP, and Pan Pacific Pressure Injury Alliance signals that this gap is being formally addressed.
For dementia caregivers, this shift matters because it is likely to drive improvements in clinical practice, equipment availability through health services, and the quality of discharge planning for patients who spend significant hours seated. Stakeholder feedback on the new guidelines remains open until February 1, 2026, through the International Guideline website, and advocacy organizations, care providers, and families are encouraged to contribute. As the evidence base for seated pressure care grows, the expectation is that individualized cushion assessment will become a standard part of dementia patient discharge protocols rather than an afterthought.
Conclusion
Choosing the right cushion for a dementia patient after hospital discharge is a clinical decision that directly affects health outcomes, readmission risk, and quality of life. The evidence is unambiguous: dementia patients face dramatically elevated risk of pressure ulcers, and pressure ulcers in this population are associated with drastically reduced survival. High-specification pressure redistributing cushions — whether foam-gel hybrids for moderate risk or alternating pressure systems for high risk — are recommended by NICE and international guidelines. Ring cushions should never be used. Covers should be waterproof yet vapor-permeable. Cushions should be regularly checked for bottoming out.
And the cushion should be selected as part of a broader seating strategy that may include tilt-in-space positioning. The most important next step for any family navigating this situation is to request an occupational therapy or tissue viability assessment as part of the hospital discharge process. Do not wait for someone to offer it. Ask for it explicitly. If that assessment has not happened and the patient is already home, contact your GP or community nursing team to arrange one. In the UK, remember that NHS intermediate care covers equipment provision for six weeks after discharge. The right cushion, properly selected and maintained, is one of the most effective and least expensive interventions available to protect a vulnerable person during one of the most dangerous transitions in their care.