Living with Parkinson’s disease and reduced stability means learning to navigate a world that suddenly feels unreliable beneath your feet. The ground hasn’t changed, but your relationship with it has””balance becomes something you must consciously negotiate rather than take for granted, and every step requires a degree of attention that most people reserve for complex tasks. For those newly diagnosed or watching a loved one struggle, the reality is that stability challenges in Parkinson’s are manageable but require significant lifestyle adjustments, consistent physical therapy, environmental modifications, and often a fundamental shift in how you approach daily movement. Consider Margaret, a 67-year-old retired teacher who was diagnosed four years ago.
She describes her morning routine as “a negotiation with gravity”””she no longer bounds out of bed but instead sits at the edge for thirty seconds, plants both feet firmly, and uses her nightstand for support as she rises. This deliberate approach has prevented falls, but it also means her mornings take twice as long as they once did. Her experience reflects what millions of Parkinson’s patients face: the disease doesn’t just affect movement, it transforms the entire rhythm of daily life. This article explores the lived experience of balance challenges in Parkinson’s disease, drawing on personal accounts and clinical insights. We’ll examine why stability becomes compromised, how people adapt their homes and routines, the role of physical therapy and assistive devices, the emotional weight of losing independence, and practical strategies that help people maintain quality of life despite these challenges.
Table of Contents
- How Does Parkinson’s Disease Affect Balance and Stability?
- The Physical Reality of Reduced Mobility in Daily Life
- Personal Accounts: What Patients Say About Losing Their Footing
- Practical Strategies for Managing Stability at Home
- When Stability Problems Signal Disease Progression
- The Role of Physical Therapy and Exercise
- Assistive Devices: Finding the Right Tools
- Looking Ahead: Research and Hope
- Conclusion
How Does Parkinson’s Disease Affect Balance and Stability?
parkinson‘s disease disrupts the brain’s ability to coordinate the complex symphony of muscle movements required for balance. The basal ganglia, a region deep in the brain responsible for motor control, loses dopamine-producing neurons, which impairs the automatic postural adjustments that healthy individuals make unconsciously hundreds of times per day. When you stand on a moving bus or step over a curb, your brain makes instantaneous calculations and micro-corrections””Parkinson’s slows and scrambles these signals. The result is what neurologists call postural instability, which typically emerges in the middle to later stages of the disease. Patients describe feeling like they’re walking on a boat deck or standing on ice.
The body’s natural protective reflexes””the quick step backward when you start to fall, the arm that shoots out to catch yourself””become delayed or absent entirely. one patient, Robert, a 72-year-old engineer, explained it this way: “My brain still knows what to do, but by the time the message reaches my legs, I’m already falling.” What makes Parkinson’s-related instability particularly challenging is its unpredictability. Symptoms can fluctuate dramatically throughout the day, influenced by medication timing, fatigue, stress, and even the environment itself. A person might walk confidently at 10 a.m. but freeze completely in a doorway by 2 p.m. This variability makes planning difficult and can lead to social isolation, as patients become reluctant to venture out when they cannot predict how their body will perform.
The Physical Reality of Reduced Mobility in Daily Life
The physical toll of living with reduced stability extends far beyond the obvious risk of falls. Patients often develop compensatory movement patterns””shuffling steps, a forward-leaning posture, or a wide-based gait””that create secondary problems including back pain, hip strain, and chronic fatigue from the constant muscular tension required to stay upright. The body works harder to accomplish less, and exhaustion becomes a constant companion. simple tasks transform into complex operations. Getting dressed requires sitting down.
Showering demands grab bars and a bench. Cooking means planning routes through the kitchen to maintain contact with counters and walls. Thomas, diagnosed at 58, gave up his woodworking hobby not because he couldn’t still operate the tools, but because standing at the workbench for extended periods became impossible. “I could make the cuts,” he said, “but I couldn’t trust myself not to stumble into the blade.” However, it’s important to note that the severity of balance problems varies enormously among patients, and some people maintain relatively good stability for many years after diagnosis. Those who remain physically active, engage in regular balance-focused exercise, and work with skilled physical therapists often fare significantly better than those who reduce activity out of fear. The instinct to move less in order to avoid falls can actually accelerate decline””the less you challenge your balance system, the faster it deteriorates.
Personal Accounts: What Patients Say About Losing Their Footing
When people with Parkinson’s describe their experience of reduced stability, the language of loss dominates. They speak of losing confidence, losing independence, and losing the person they used to be. Patricia, a 70-year-old former dancer, said that giving up her spontaneity was harder than giving up dancing itself. “I used to jump up and go wherever I wanted,” she recalled. “Now I have to think about every step. It’s exhausting in a way that has nothing to do with physical tiredness.” The psychological burden of constant vigilance weighs heavily on patients. Many describe a mental fatigue that compounds the physical challenges””the brain simply isn’t designed to consciously manage processes that should be automatic.
Sleep suffers because even rolling over in bed requires deliberate effort. Conversations become difficult to follow because part of the mind is always monitoring body position. The cognitive load of living with instability leaves less mental energy for everything else. James, a 65-year-old who has lived with Parkinson’s for seven years, offered a particularly vivid account: “Imagine you’re walking across a log over a stream, and you have to focus completely on every step. Now imagine that’s every hallway, every sidewalk, every trip to the bathroom at night. That’s my life now. The fear isn’t about one fall””it’s about knowing that the next ten thousand steps all carry risk.” His words capture the relentless nature of stability challenges, the way they transform not just movement but consciousness itself.
Practical Strategies for Managing Stability at Home
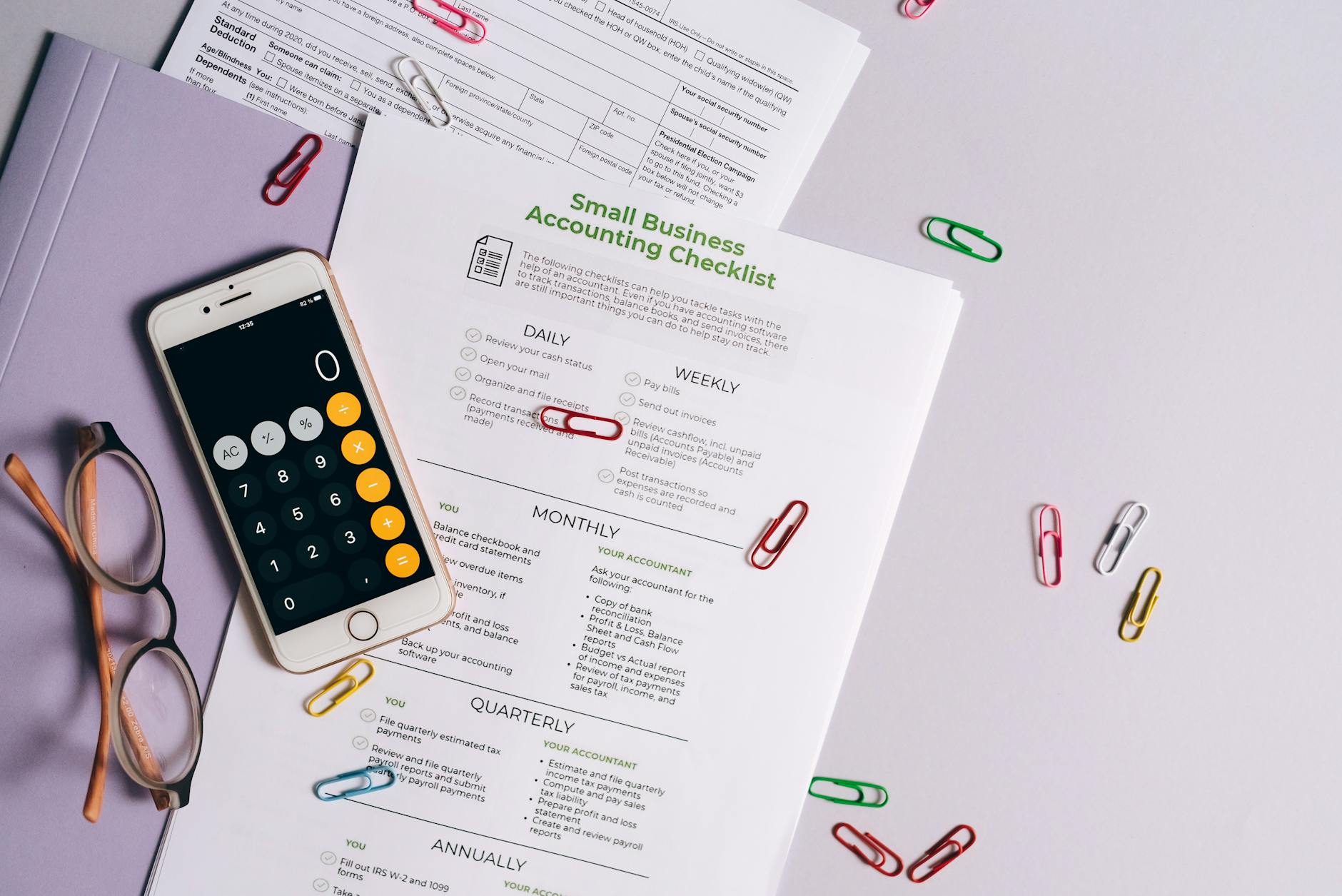
Home modification is one of the most effective interventions for people living with Parkinson’s-related balance problems, yet many families delay these changes until after a serious fall. Occupational therapists recommend proactive assessment””ideally within the first year of diagnosis””to identify hazards and implement solutions before they become urgent. The goal is creating an environment that compensates for impaired balance without making the home feel like a medical facility. Grab bars in bathrooms, non-slip flooring, removal of throw rugs, adequate lighting, and furniture arranged to provide continuous support paths are foundational modifications. More advanced adaptations include stairlifts, walk-in tubs or roll-in showers, raised toilet seats, and motion-activated lighting for nighttime navigation.
The tradeoff with many of these modifications is between safety and aesthetics””some patients resist changes that make their homes look “institutional,” while others embrace any modification that allows them to remain in their own space rather than moving to assisted living. The comparison between minimal and comprehensive home modification is stark in outcome data. Studies suggest that patients who implement full environmental modifications experience up to 40% fewer falls than those who make only minor changes. However, modifications alone are insufficient””they must be combined with behavioral changes. The most sophisticated grab bar helps nothing if the patient doesn’t use it, and old habits of rushing through familiar spaces take conscious effort to break.
When Stability Problems Signal Disease Progression
Worsening balance often serves as a marker for Parkinson’s progression, and patients understandably become anxious when they notice changes. However, it’s crucial to distinguish between disease advancement and other treatable causes of declining stability. Medication adjustments, infections, dehydration, blood pressure fluctuations, vision changes, and depression can all worsen balance without indicating actual neurological decline. A sudden change in stability should always prompt medical evaluation rather than resignation. The timing of stability problems relative to other Parkinson’s symptoms carries prognostic significance. When significant balance impairment appears early in the disease course””within the first few years of motor symptoms””it may indicate a Parkinson’s-plus syndrome such as progressive supranuclear palsy (PSP) or multiple system atrophy (MSA), conditions that typically progress more rapidly and respond less well to standard Parkinson’s medications.
This is why accurate diagnosis matters: the treatment approach and prognosis differ considerably. Patients should be warned that not every fall represents a turning point. Eleanor, now 75, had three falls in one month and assumed her disease had dramatically worsened. Her neurologist discovered she had developed a urinary tract infection that was causing confusion and unsteadiness””once treated with antibiotics, her balance returned to its previous baseline. “I had already started planning for a nursing home in my head,” she admitted. “It turned out to be something completely fixable.”.

The Role of Physical Therapy and Exercise
Physical therapy specifically targeting balance is among the most evidence-supported interventions for Parkinson’s-related stability problems. Programs that incorporate LSVT BIG (a specialized amplitude-based approach), tai chi, dance therapy, or boxing-inspired training have all demonstrated benefits in clinical trials. The key principle across these approaches is challenging the balance system in a controlled environment, forcing the brain to rebuild or maintain the neural pathways responsible for postural control. Martha, a 69-year-old patient, described her twice-weekly physical therapy sessions as “the most important appointment on my calendar.” She initially resisted the exercises, which seemed impossibly difficult””standing on one foot, walking heel-to-toe, catching a ball while balancing on a foam pad. “I felt ridiculous and frustrated,” she said.
“But six months in, I realized I hadn’t fallen once. Before PT, I was falling every few weeks.” Her experience aligns with research showing that consistent, challenging balance work can significantly reduce fall frequency. The limitation of physical therapy is that benefits require ongoing maintenance””they don’t accumulate permanently like money in a savings account. Patients who stop exercising typically see their gains erode within weeks to months. This means that effective management of Parkinson’s-related stability problems requires a permanent commitment to physical activity, which can feel overwhelming for people already struggling with fatigue and motivation. Finding enjoyable forms of exercise, building routines, and enlisting accountability partners all help sustain engagement.
Assistive Devices: Finding the Right Tools
The range of assistive devices for balance problems extends from simple canes to sophisticated wheeled walkers with laser guides that help patients overcome freezing episodes. Choosing the right device involves balancing functionality, stigma, and individual symptom patterns. Many patients resist devices because they symbolize disability, while others embrace them for the independence they restore. There’s no universal right answer””the best device is the one that gets used. Rollator walkers with four wheels, hand brakes, and a seat have become popular among Parkinson’s patients because they provide substantial support while remaining maneuverable.
Some models now include laser lines that project onto the floor, giving the brain a visual target that can help overcome freezing. The comparison between standard and laser-equipped rollators is notable: small studies suggest the laser feature reduces freezing episodes by roughly half in patients for whom freezing is a primary problem. William, diagnosed at 62, held off on using a walker for two years, relying on furniture and walls for support at home and avoiding outings where support wasn’t available. When he finally tried a rollator, his reaction surprised him: “I felt like I got my life back. I was so worried about looking old or sick, but nobody cares about my walker””they just see me at the grocery store, at the park, living my life again.” His regret was waiting so long.
Looking Ahead: Research and Hope
Research into Parkinson’s balance problems is advancing on multiple fronts. Deep brain stimulation (DBS), already used to treat tremor and rigidity, is being refined to better address gait and balance””newer stimulation targets and adaptive programming show promise. Wearable technology that detects subtle changes in gait patterns may soon provide early warning of impending falls, allowing preventive intervention. Gene therapies and disease-modifying treatments, though still largely experimental, aim to slow or halt neurodegeneration itself.
For patients living with reduced stability today, hope lies not only in future breakthroughs but in the substantial improvements possible with current approaches. Optimized medication regimens, consistent physical therapy, appropriate assistive devices, home modification, and psychological support can collectively transform quality of life. The disease remains incurable, but the experience of living with it is far from fixed””proactive management makes a genuine difference. As one patient summarized: “Parkinson’s took a lot from me, but it didn’t take everything. I still decide how I respond to it.”.
Conclusion
Living with Parkinson’s-related balance problems demands adaptation at every level””physical, environmental, emotional, and social. The accounts shared here reveal both the profound challenges of reduced stability and the resilience that patients develop in response. Falls and fear need not define the experience; with proper support, many people maintain meaningful independence and quality of life for years after balance problems emerge.
The path forward involves assembling a comprehensive support team, including neurologists, physical therapists, occupational therapists, and often mental health professionals, while simultaneously making practical changes to daily routines and living spaces. Most importantly, it requires accepting help and assistive devices not as symbols of defeat but as tools for continued engagement with life. The ground may feel less reliable, but solid footing is still possible””it just takes more effort, more planning, and more willingness to ask for support.





