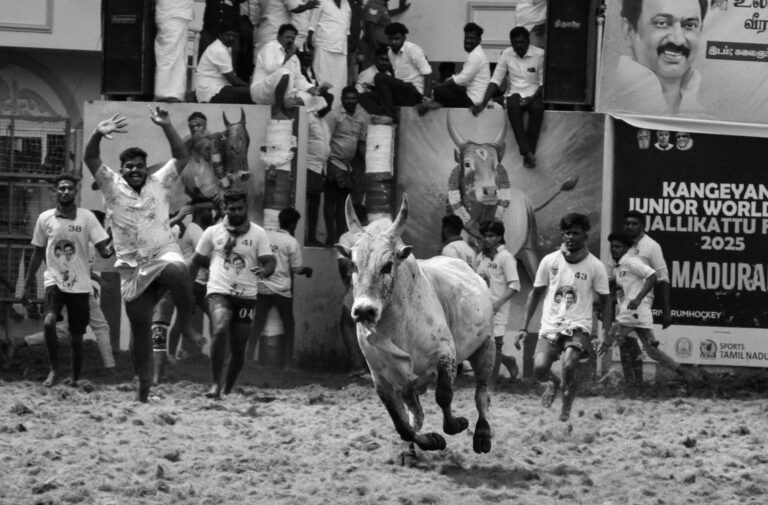
Parkinson’s disease transforms ordinary floors, carpets, and thresholds into genuine safety threats through its progressive erosion of motor control, balance, and spatial perception. The neurological changes that characterize Parkinson’s””including bradykinesia (slowed movement), rigidity, postural instability, and gait disturbances like shuffling and freezing””mean that a surface transition most people cross without thinking can trigger a fall. A simple change from hardwood to a rug, a slightly raised doorway threshold, or even a shift in floor color can cause someone with Parkinson’s to freeze mid-step or lose their balance entirely. Consider a retired teacher who navigated her home for forty years without incident.
After her Parkinson’s diagnosis, the decorative area rug in her living room became a recurring fall site. Her shuffling gait caught on the rug’s edge repeatedly, and the visual contrast between the rug and the surrounding floor triggered freezing episodes that left her stranded mid-step. What had been a cherished decor choice became a source of injury and anxiety””a pattern that plays out in households across the world as Parkinson’s fundamentally changes how people interact with their physical environment. This article examines why these surface-related hazards develop, which specific features pose the greatest risks, and what practical modifications can reduce fall danger. We will also explore the role of visual perception changes, the limitations of common solutions, and emerging approaches that may help people with Parkinson’s move more safely through their homes.
Table of Contents
- Why Does Parkinson’s Disease Make Normal Floors Dangerous?
- The Hidden Role of Visual Perception in Surface-Related Falls
- Which Household Surfaces Pose the Greatest Fall Risk?
- How Can Home Modifications Reduce Surface Hazards?
- When Do Standard Safety Measures Fall Short?
- The Role of Mobility Aids on Different Surfaces
- Future Directions in Surface Safety for Parkinson’s Disease
- Conclusion
Why Does Parkinson’s Disease Make Normal Floors Dangerous?
The danger lies in how Parkinson’s disrupts the complex neurological processes that govern walking. Healthy gait involves automatic adjustments””lifting feet to clear obstacles, shifting weight smoothly, and maintaining balance through subtle postural corrections. The basal ganglia, the brain region most affected by Parkinson’s, plays a central role in automating these movements. When dopamine-producing neurons in this region degenerate, movements that were once unconscious require deliberate effort, and many adjustments simply fail to happen. Shuffling gait, one of Parkinson’s hallmark symptoms, creates particular problems with surface transitions. Instead of lifting feet and placing them down with adequate clearance, people with Parkinson’s often slide their feet forward in small steps.
This means even minor surface irregularities””a carpet edge raised by a quarter inch, a threshold strip, or uneven tile””can catch the foot and cause a trip. Research has historically indicated that falls are among the most common complications of Parkinson’s, with some studies suggesting that over two-thirds of people with the condition experience at least one fall per year. Freezing of gait compounds these risks dramatically. During a freezing episode, a person’s feet seem glued to the floor despite their intention to move. These episodes are frequently triggered by environmental factors: doorways, narrow passages, and transitions between different floor surfaces. Someone might walk smoothly across an open room, then freeze completely when approaching the kitchen doorway or stepping from tile onto carpet. The unpredictability of freezing makes it particularly hazardous, as it can occur mid-stride and lead to a forward fall.
The Hidden Role of Visual Perception in Surface-Related Falls
parkinson‘s disease affects more than motor function””it also impairs visual processing in ways that make surfaces deceptively dangerous. Many people with Parkinson’s experience reduced contrast sensitivity, difficulty with depth perception, and slower visual processing speeds. These changes mean that distinguishing between a shadow on the floor and an actual step, or perceiving the edge of a rug against similar-colored flooring, becomes genuinely difficult. Visual perception problems help explain why high-contrast floor patterns can trigger freezing episodes. Striped patterns, checkerboard tiles, or even strong shadows cast across a walkway may be misinterpreted as obstacles or changes in floor level. The brain, already struggling with motor planning, receives confusing visual information that further disrupts movement.
Some people report that dark doormats appear as holes in the floor, causing them to hesitate or attempt to step over them in ways that throw off their balance. However, visual challenges also point toward potential solutions. While busy patterns and poor lighting exacerbate problems, strategic use of visual cues can actually help. Horizontal lines or colored tape placed perpendicular to the direction of travel have been shown to reduce freezing in many cases by providing a stepping target. This works only when the visual cue is clearly distinct from the surrounding environment””a limitation that means what helps one person may be ineffective or even counterproductive for another. Individual assessment and experimentation remain essential.
Which Household Surfaces Pose the Greatest Fall Risk?
Not all surfaces are equally dangerous. Certain features appear consistently in fall reports and clinical observations, though individual sensitivity varies considerably. Loose rugs and mats rank among the highest-risk items because they combine multiple hazards: raised edges that catch shuffling feet, potential for sliding on smooth floors, and visual boundaries that may trigger freezing. Even rugs secured with non-slip backing can present problems if their edges curl or if the visual contrast with surrounding flooring is too stark. Thresholds and floor transitions present another major category of risk. The metal strips between rooms, raised doorway sills, and changes between flooring materials all require the kind of deliberate step adjustment that Parkinson’s makes difficult.
A transition from bathroom tile to bedroom carpet might involve both a slight height change and a dramatic texture difference””each element demanding attention from a motor system already operating at reduced capacity. Wet bathroom floors add another layer of danger, as both moisture and the glossy appearance of wet tile increase slip and fall risk. Outdoor surfaces introduce additional variables. Uneven sidewalks, gravel paths, grass, and inclined driveways all challenge balance systems already compromised by Parkinson’s. Weather-related changes””wet leaves, ice, or even damp pavement””can make familiar paths unpredictable. One specific example from clinical literature describes a man who walked his driveway daily for years, only to begin falling regularly after his Parkinson’s progressed. The slight slope he had never noticed became a significant challenge when his postural reflexes could no longer compensate automatically.

How Can Home Modifications Reduce Surface Hazards?
Modifying the home environment represents one of the most effective strategies for reducing fall risk, though no modification eliminates danger entirely. The foundational approach involves removing or securing anything that could catch feet or cause slipping. This means removing loose rugs or replacing them with firmly secured, low-pile alternatives. Area rugs with raised edges should be eliminated entirely, as the tripping risk outweighs any aesthetic or comfort benefit. Floor transitions can often be addressed by installing beveled threshold strips that create a gradual slope rather than an abrupt edge. In some cases, removing thresholds entirely and using flexible transition strips that sit nearly flush with both surfaces offers a better solution.
When replacing flooring, choosing consistent surfaces throughout main living areas eliminates many transition points””though this represents a significant investment and disruption that isn’t feasible for everyone. For bathrooms, textured non-slip flooring or large-format non-slip mats that cover most of the floor surface can reduce wet-surface danger. The tradeoff with many modifications involves balancing safety against independence and quality of life. Removing all rugs may reduce fall risk but also eliminates warmth, sound absorption, and familiar comfort. Installing grab bars throughout the home provides security but may feel institutional. The most successful approaches typically involve occupational therapy assessment to identify individual-specific risks and preferences, then implementing modifications that address the highest-priority hazards while respecting the person’s home environment and autonomy.
When Do Standard Safety Measures Fall Short?
Standard home safety recommendations have significant limitations when applied to Parkinson’s disease. Generic fall-prevention advice””keep pathways clear, use non-slip mats, install handrails””addresses some concerns but misses Parkinson’s-specific challenges. A clear pathway doesn’t help when freezing occurs in open spaces. Non-slip mats can themselves become tripping hazards or freezing triggers. Handrails provide support but don’t address the gait disturbances that initiate falls. One critical limitation involves the progressive nature of Parkinson’s. Modifications that work well during early and middle stages may become insufficient as the disease advances.
A person who safely navigated their modified home for years may suddenly begin falling again as motor symptoms worsen or medication effectiveness fluctuates. The “on-off” phenomenon””where medication effects wear off unpredictably””means that environmental hazards a person handles easily during “on” periods become dangerous during “off” periods. This variability makes it impossible to establish a single set of modifications that works at all times. Cognitive changes that often accompany Parkinson’s further complicate matters. Executive function decline can impair judgment about when to use mobility aids or ask for help. Dementia, which develops in a substantial portion of people with Parkinson’s over time, may make it impossible to remember and follow safety strategies. Visual cueing techniques that require conscious attention become less effective as cognitive resources diminish. Families and caregivers should anticipate the need for ongoing reassessment and modification as the disease progresses.

The Role of Mobility Aids on Different Surfaces
Mobility aids interact with surfaces in ways that can either improve or worsen safety. Standard walkers provide stability on smooth, flat surfaces but can catch on thresholds and carpet edges. Wheeled walkers roll more easily but may accelerate unexpectedly on slopes or slick floors. Canes offer less support but greater maneuverability in tight spaces where freezing commonly occurs.
The choice of mobility aid often requires surface-by-surface thinking. Some people use a rollator walker throughout most of their home but switch to a cane for navigating the small bathroom where the walker doesn’t fit. Others find that wheeled walkers actually worsen their safety on carpet because the resistance difference between carpet and hard flooring disrupts their rhythm. Laser canes, which project a line on the floor to help overcome freezing, work well for some individuals but have no benefit for those whose freezing isn’t visually triggered.
Future Directions in Surface Safety for Parkinson’s Disease
Emerging technologies and research offer potential improvements in managing surface-related hazards, though widespread availability and proven effectiveness remain limited. Wearable devices that detect freezing episodes and provide rhythmic auditory or vibration cues are under development and have shown promise in research settings. Smart home systems that could automatically adjust lighting to improve surface visibility or alert caregivers to falls represent another area of active investigation.
Research into the neurological mechanisms of freezing and gait disturbance continues to advance understanding of why surfaces trigger problems. This knowledge may eventually lead to more targeted interventions, whether through medication adjustments, deep brain stimulation programming, or rehabilitation techniques. For now, the combination of thoughtful home modification, regular occupational therapy reassessment, appropriate mobility aids, and caregiver education remains the most effective approach to reducing the dangers that everyday surfaces pose to people living with Parkinson’s disease.
Conclusion
Parkinson’s disease fundamentally alters the relationship between a person and their physical environment, turning unremarkable floors, thresholds, and surface transitions into genuine hazards. The combination of shuffling gait, freezing episodes, postural instability, and visual perception changes means that fall prevention requires understanding these specific mechanisms rather than applying generic safety advice. Recognizing which surfaces pose the greatest risk””loose rugs, abrupt transitions, high-contrast patterns, wet floors””allows for targeted modification.
Effective management requires ongoing attention and adaptation. Home modifications that address current hazards should be combined with regular reassessment as the disease progresses and symptoms change. Working with occupational therapists, physical therapists, and neurologists helps ensure that environmental strategies complement medical management. While no approach eliminates fall risk entirely, thoughtful attention to surface hazards can meaningfully reduce injuries and help people with Parkinson’s maintain independence and safety in their own homes.