Parkinson’s disease transforms an active lifestyle through a gradual but relentless erosion of motor control, beginning with subtle tremors or stiffness that make familiar activities increasingly difficult, then progressing to affect balance, coordination, and the automatic movements most people take for granted. For someone who once hiked mountain trails, played tennis on weekends, or simply walked briskly through the neighborhood, the disease introduces a new reality where every physical action requires conscious effort and careful planning. The dopamine-producing neurons that once seamlessly coordinated movement deteriorate over time, and the body that responded instinctively to the brain’s commands begins to hesitate, freeze, or move in ways that feel foreign. Consider a former marathon runner who notices her arm no longer swings naturally when she walks, or a retired carpenter whose hands now shake too much to hold tools steady.
These individuals don’t lose their desire for activity””they lose the reliable partnership between intention and execution that makes activity possible. The psychological toll compounds the physical challenges, as activities that once defined identity and brought joy become sources of frustration or even danger. This article explores the specific ways Parkinson’s disease reshapes physical capability, examines which activities become most challenging and why, discusses adaptive strategies that help maintain meaningful movement, and addresses the emotional journey of accepting a fundamentally changed relationship with one’s body. Understanding these transformations helps patients, caregivers, and families navigate the transition with greater knowledge and realistic expectations.
Table of Contents
- What Happens to Physical Abilities When Parkinson’s Disease Develops?
- Why Balance and Coordination Deteriorate Over Time
- The Psychological Impact of Losing Physical Independence
- When Standard Treatments Stop Working Effectively
- Adapting Homes and Routines for Safer Living
- Looking Ahead: Emerging Research and Future Possibilities
- Conclusion
What Happens to Physical Abilities When Parkinson’s Disease Develops?
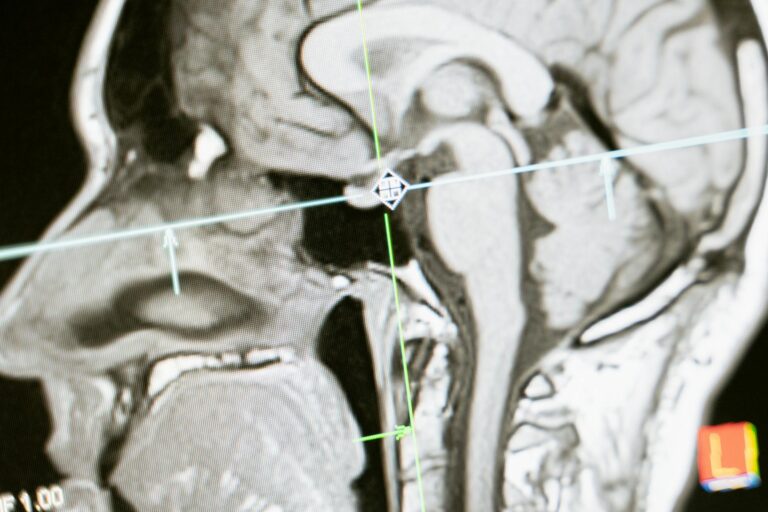
The motor symptoms of Parkinson’s disease emerge because the brain loses cells in the substantia nigra, a region responsible for producing dopamine. This neurotransmitter acts as a messenger that helps coordinate smooth, controlled movements. When dopamine levels drop, the brain struggles to send clear signals to muscles, resulting in the cardinal symptoms: tremor at rest, rigidity or stiffness, bradykinesia (slowness of movement), and postural instability. These symptoms rarely appear all at once; typically, they develop on one side of the body first and gradually spread over months or years. For an active person, bradykinesia often proves most disruptive to daily life. Actions that once happened automatically””buttoning a shirt, typing an email, or walking across a room””now require deliberate focus and take longer to complete.
A former cyclist might find that initiating pedaling becomes difficult, or that his legs feel frozen at traffic lights. The disease doesn’t cause paralysis; the muscles still work, but the neural pathways that trigger and sustain movement become unreliable. This creates a frustrating disconnect where the mind remains capable but the body fails to respond appropriately. Rigidity adds another layer of difficulty by making muscles feel tight and inflexible, even at rest. Unlike typical muscle soreness that improves with stretching, Parkinson’s rigidity stems from neurological dysfunction and persists regardless of physical therapy. Combined with tremor””which affects roughly 70% of patients and typically worsens during stress or fatigue””these symptoms collectively transform how a person interacts with the physical world. Activities that once built fitness and confidence now require careful risk assessment and adaptation.

Why Balance and Coordination Deteriorate Over Time
Balance problems represent one of the most dangerous aspects of Parkinson’s disease progression, typically emerging in the middle to later stages. The disease affects the brain’s ability to make rapid postural adjustments, meaning patients struggle to catch themselves when they start to fall. Healthy individuals unconsciously shift weight, adjust their stance, and engage stabilizing muscles dozens of times per minute; Parkinson’s patients lose this automatic protective system. Falls become significantly more likely and more consequential. Research indicates that approximately 60% of Parkinson’s patients experience at least one fall per year, and many fall repeatedly.
The consequences extend beyond immediate injury””hip fractures, head trauma, and other fall-related injuries frequently lead to hospitalization, loss of independence, and accelerated decline. Fear of falling creates its own problem: patients may restrict their activities so severely that deconditioning worsens their overall mobility, creating a downward spiral. However, if balance problems are caught early and addressed with targeted physical therapy, patients can often maintain safer mobility for longer periods. Specific exercises that challenge balance””like tai chi, which has shown particular effectiveness in Parkinson’s research””can help the brain develop compensatory strategies. The limitation is that exercise cannot stop disease progression; it can only optimize function within the constraints of neurological damage. Patients who were highly active before diagnosis often retain better baseline strength and coordination, but even they will eventually face significant balance challenges as the disease advances.
The Psychological Impact of Losing Physical Independence
Adapting to Parkinson’s disease involves mourning the loss of a former self. For individuals whose identities centered on physical capability””athletes, dancers, outdoor enthusiasts, or simply active parents and grandparents””the disease forces a fundamental redefinition of who they are. Depression affects approximately 40% of Parkinson’s patients, and anxiety disorders affect a similar proportion. These aren’t simply reactions to difficult circumstances; the same dopamine deficiency that causes motor symptoms also disrupts mood-regulating neural circuits. A retired firefighter who spent decades relying on his physical strength and quick reflexes may find himself unable to walk across an icy parking lot without assistance. A grandmother who loved chasing her grandchildren at the park may now watch from a bench, afraid that running would send her tumbling. These losses accumulate, and the grief is real. Social isolation often follows, as patients withdraw from activities where their symptoms feel conspicuous or where they fear being a burden. Cognitive changes compound emotional challenges in some patients. Parkinson’s disease dementia eventually affects roughly 50% of patients, though timing varies widely. Even before dementia develops, many patients experience slower thinking, difficulty with multitasking, and problems with executive function””the mental processes that help plan and execute complex activities.
For someone already struggling with motor symptoms, adding cognitive challenges makes adapting to new realities even harder. ## How to Maintain Physical Activity with Parkinson’s Disease Continuing physical activity remains one of the most effective interventions for managing Parkinson’s disease, though the type and intensity of activity must evolve with the condition. Exercise appears to have neuroprotective effects and consistently improves motor symptoms, mood, and quality of life in research studies. The challenge lies in finding sustainable activities that accommodate changing abilities while still providing meaningful physical engagement. Structured exercise programs designed specifically for Parkinson’s patients offer several advantages over independent workouts. Programs like Rock Steady Boxing (a non-contact boxing fitness program adapted for Parkinson’s) provide supervised, progressive training in environments where participants share similar challenges. Aquatic exercise reduces fall risk while allowing resistance training, and cycling””particularly on stationary bikes or tandems””leverages the relatively preserved ability to perform rhythmic, continuous movements. The tradeoff is that specialized programs aren’t available everywhere, may involve costs not covered by insurance, and require transportation that becomes problematic as the disease progresses. Home-based exercise offers accessibility but demands more self-discipline and often provides less optimal results without professional guidance. Physical therapists with Parkinson’s expertise can design individualized programs, but insurance limitations often restrict the number of covered sessions. Technology-based solutions like video-guided exercise programs or virtual reality systems show promise but remain relatively unproven compared to in-person supervision. Whatever approach patients choose, consistency matters more than intensity””regular moderate activity typically outperforms sporadic vigorous efforts.

When Standard Treatments Stop Working Effectively
Medication management becomes increasingly complex as Parkinson’s disease progresses. Levodopa, the gold-standard treatment, works by supplementing the brain’s depleted dopamine supply. Early in the disease, it typically provides smooth, reliable symptom control. Over time, however, patients often develop motor fluctuations””periods when medication works well (called “on” time) alternating unpredictably with periods when symptoms return (called “off” time). These fluctuations make planning physical activity extremely difficult. Dyskinesias present another challenge. These involuntary, often writhing movements paradoxically result from medication rather than the disease itself, typically appearing after years of levodopa use.
Patients face an impossible choice: take enough medication to move adequately and risk dyskinesias, or take less and remain stiff and slow. Neither option restores normal movement. Some patients describe their day as a narrow window when medication levels align perfectly and activity feels possible, bookended by hours of either frozen immobility or uncontrollable movement. Deep brain stimulation surgery offers hope for some patients whose medication no longer provides adequate control. This procedure involves implanting electrodes in specific brain regions and using electrical pulses to modulate abnormal neural activity. The limitation is significant: not all patients qualify, the surgery carries risks including infection and cognitive effects, and it works best for motor fluctuations and dyskinesias rather than balance problems or freezing of gait. Surgery also doesn’t halt disease progression””it optimizes the brain’s response to available dopamine but cannot restore what’s been lost.
Adapting Homes and Routines for Safer Living
Environmental modifications can significantly extend how long Parkinson’s patients safely maintain independence. Simple changes””removing throw rugs, improving lighting, installing grab bars in bathrooms, and rearranging furniture to create clear walking paths””reduce fall risk without requiring major renovations.
Occupational therapists specialize in evaluating homes and recommending practical modifications tailored to individual needs. A former tennis player who now experiences freezing episodes (sudden, temporary inability to move, especially when approaching doorways or starting to walk) might benefit from visual cues on the floor””strips of tape placed at regular intervals can help the brain restart movement by providing targets to step over. The same technique helps some patients navigate crowded or narrow spaces where freezing commonly occurs.

Looking Ahead: Emerging Research and Future Possibilities
Research into Parkinson’s disease has accelerated in recent years, with multiple promising approaches in various stages of investigation. Gene therapies aim to slow neurodegeneration or help remaining brain cells compensate for lost dopamine production. Stem cell research explores whether transplanting dopamine-producing cells could restore function.
Exercise scientists are developing more precise protocols to maximize neuroprotective benefits. None of these approaches currently offers a cure, and realistic expectations remain essential. However, the combination of better symptomatic treatments, improved surgical techniques, and potentially disease-modifying therapies may mean that patients diagnosed today face a different trajectory than those diagnosed decades ago. The goal for active individuals with Parkinson’s isn’t necessarily to maintain their exact former lifestyle””it’s to preserve as much meaningful physical engagement as possible for as long as possible while adapting to inevitable changes.
Conclusion
Parkinson’s disease fundamentally transforms how active individuals relate to their bodies and their favorite activities. The progressive loss of dopamine-producing neurons disrupts the seamless connection between intention and movement, making once-automatic actions difficult, unpredictable, or impossible. Balance deteriorates, medication effects fluctuate, and psychological challenges compound physical ones. For people who defined themselves through physical capability, these changes require grieving a former identity while building a new one.
Yet meaningful physical activity remains both possible and beneficial throughout most of the disease course. Adapted exercise programs, environmental modifications, skilled medical management, and psychological support can help maintain quality of life even as capabilities change. The key lies in accepting that active living will look different””not necessarily worse, but different””and working with healthcare providers, therapists, and support networks to optimize what remains possible. Starting these adaptations early, before crisis forces change, gives patients the best chance of preserving what matters most about their active lives.