Understanding why early amyloid detection matters for treatment has become one of the most critical conversations in modern neurology and dementia care. Amyloid plaques””abnormal protein deposits that accumulate in the brain””are among the earliest detectable signs of Alzheimer’s disease, often appearing decades before the first symptoms of cognitive decline. This silent buildup creates a window of opportunity that researchers and clinicians are only now learning to leverage effectively. The urgency surrounding early detection stems from a fundamental shift in how the medical community approaches Alzheimer’s disease. For decades, treatment options were limited to managing symptoms after significant brain damage had already occurred.
Today, a new generation of disease-modifying therapies targets amyloid directly, but these treatments show the greatest promise when administered before extensive neurodegeneration takes hold. The difference between detecting amyloid buildup at age 55 versus age 70 could mean the difference between maintaining independence and requiring full-time care. This article explores the science behind amyloid accumulation, the technologies enabling earlier detection, and the practical implications for patients and families navigating these decisions. By the end, readers will understand the biological rationale for early intervention, the current state of diagnostic tools, and concrete steps for discussing amyloid testing with healthcare providers. The goal is not to create alarm but to provide the information needed to make informed choices about brain health monitoring and potential treatment pathways.
Table of Contents
- What Is Amyloid and Why Does Early Detection Matter for Alzheimer’s Treatment?
- How Amyloid Biomarkers Transform Alzheimer’s Diagnosis and Treatment Planning
- The Therapeutic Window: When Treatment Timing Impacts Outcomes
- Practical Steps for Pursuing Early Amyloid Testing
- Challenges and Controversies in Early Amyloid Detection Programs
- Emerging Technologies Advancing Early Amyloid Detection Methods
- How to Prepare
- How to Apply This
- Expert Tips
- Conclusion
- Frequently Asked Questions
What Is Amyloid and Why Does Early Detection Matter for Alzheimer’s Treatment?
amyloid beta is a protein fragment that occurs naturally in the brain, typically cleared away by normal cellular processes. In Alzheimer’s disease, this clearance mechanism fails, allowing amyloid fragments to clump together and form plaques between neurons. These plaques disrupt cell-to-cell communication, trigger inflammatory responses, and eventually contribute to the death of brain cells. The process unfolds slowly””current research suggests amyloid accumulation begins 15 to 20 years before noticeable memory problems emerge. Early detection matters because the brain has remarkable capacity for compensation during the initial phases of amyloid buildup.
Cognitive reserve””the brain’s ability to improvise and find alternate routes for completing tasks””allows many people to function normally despite growing pathology. However, this compensation has limits. Once symptoms appear, substantial neuronal loss has already occurred, and lost neurons cannot be regenerated. Identifying amyloid accumulation during the presymptomatic phase opens the door to intervention before irreversible damage accumulates. The clinical significance extends beyond individual patients to broader public health considerations:.
- Treatment efficacy declines with disease progression, making early-stage intervention far more cost-effective than late-stage care management
- Early detection allows families more time for planning, including financial preparation, care arrangements, and participation in clinical trials
- Population-level screening could identify high-risk individuals for preventive measures, even before amyloid-targeting drugs are prescribed
- Research into disease mechanisms benefits from studying patients across all stages, including the presymptomatic window

How Amyloid Biomarkers Transform Alzheimer’s Diagnosis and Treatment Planning
The diagnostic landscape for Alzheimer’s disease has been revolutionized by biomarker testing. Traditional diagnosis relied heavily on clinical observation””documenting memory complaints, administering cognitive assessments, and ruling out other causes of dementia. This approach could only confirm Alzheimer’s with certainty through autopsy. Biomarker testing changes that equation entirely, allowing clinicians to detect the disease’s biological fingerprint in living patients.
Two primary methods dominate current amyloid detection: positron emission tomography (PET) imaging and cerebrospinal fluid (CSF) analysis. PET scans use radioactive tracers that bind specifically to amyloid plaques, producing images that show the location and extent of accumulation throughout the brain. CSF testing measures amyloid beta levels in spinal fluid””paradoxically, lower levels in the fluid indicate higher levels in the brain, as the protein becomes sequestered in plaques rather than circulating freely. Both methods demonstrate high accuracy for detecting amyloid pathology, though they differ in accessibility, cost, and invasiveness. Blood-based biomarkers represent the newest frontier in amyloid detection:.
- Plasma amyloid beta ratios can now predict brain amyloid status with approximately 85-90% accuracy
- Blood tests for phosphorylated tau proteins provide complementary information about disease progression
- These tests cost a fraction of PET scans and require only a standard blood draw
- Widespread availability could enable routine screening in primary care settings within the coming years
- Current limitations include variability between testing platforms and the need for further validation across diverse populations
The Therapeutic Window: When Treatment Timing Impacts Outcomes
Clinical trial data has consistently demonstrated that disease-modifying treatments perform differently depending on when they are administered. The recently approved anti-amyloid antibodies””lecanemab and donanemab””showed their strongest effects in patients with mild cognitive impairment or early-stage dementia. Patients with more advanced disease experienced less benefit and higher rates of adverse events. This pattern underscores a principle that neurologists have long suspected: the therapeutic window for Alzheimer’s intervention is narrower than previously hoped.
The biological explanation involves the cascade of events that amyloid accumulation triggers. Amyloid plaques appear first, followed by tau tangles, neuroinflammation, synaptic dysfunction, and finally neuronal death. Removing amyloid after tau pathology has become widespread and neurons have died cannot reverse the damage already done. The goal of early treatment is to interrupt this cascade before downstream effects become dominant. Think of it as addressing a water leak before it causes structural damage””stopping the water helps, but it cannot un-rot wood that has already deteriorated.
- Patients treated at the mild cognitive impairment stage showed 27-35% slowing of cognitive decline in pivotal trials
- Those with moderate dementia showed minimal to no statistical benefit from the same treatments
- Side effects, particularly amyloid-related imaging abnormalities (ARIA), occurred more frequently in advanced cases
- Genetic factors, especially APOE4 carrier status, influence both disease progression and treatment response timing

Practical Steps for Pursuing Early Amyloid Testing
Accessing amyloid testing requires navigation through healthcare systems that are still adapting to these diagnostic advances. Not all physicians are familiar with biomarker testing protocols, and insurance coverage remains inconsistent. However, multiple pathways exist for individuals concerned about their brain health or with family histories of Alzheimer’s disease.
The first step involves an honest conversation with a primary care physician about cognitive concerns and family history. Doctors can administer brief screening tools to establish a baseline and determine whether specialist referral is warranted. Neurologists and memory clinic specialists have greater familiarity with biomarker testing and can order PET scans or CSF analysis when clinically appropriate. For those without current symptoms but elevated risk factors, some academic medical centers offer research programs that include amyloid screening as part of observational studies.
- Memory clinics at major medical centers offer comprehensive evaluation including biomarker assessment
- Clinical trials frequently provide free diagnostic testing in exchange for study participation
- Direct-to-consumer blood tests are emerging, though results should always be reviewed with a qualified physician
- Insurance coverage for PET scans typically requires documented cognitive symptoms; CSF testing may face fewer restrictions
- Out-of-pocket costs for PET imaging range from $3,000 to $6,000; blood tests cost significantly less but may not yet be covered by insurance
Challenges and Controversies in Early Amyloid Detection Programs
Despite the compelling rationale for early detection, significant debates continue within the medical community about population-level screening. Critics raise legitimate concerns about the psychological impact of identifying amyloid pathology in cognitively normal individuals. Not everyone with amyloid plaques will develop dementia during their lifetime””some estimates suggest 20-30% of amyloid-positive individuals remain cognitively stable into advanced age. Telling someone they have brain pathology associated with Alzheimer’s carries weighty implications even when symptoms may never materialize.
The healthcare system’s readiness for widespread amyloid screening also raises practical concerns. Current anti-amyloid treatments require regular infusions, frequent MRI monitoring for side effects, and careful patient selection. Scaling these interventions to meet the demand created by population screening would strain already stretched neurology practices and imaging centers. Furthermore, the treatments themselves carry meaningful risks””ARIA can cause brain swelling or microhemorrhages, occasionally producing serious symptoms.
- Psychological distress following positive amyloid results has been documented, though severe reactions appear uncommon
- Some individuals report relief at having an explanation for subtle changes they had noticed
- Genetic counseling models may offer frameworks for delivering amyloid results responsibly
- The absence of preventive interventions for amyloid-positive but asymptomatic individuals creates difficult ethical terrain
- Disparities in access to testing and treatment risk widening existing health equity gaps

Emerging Technologies Advancing Early Amyloid Detection Methods
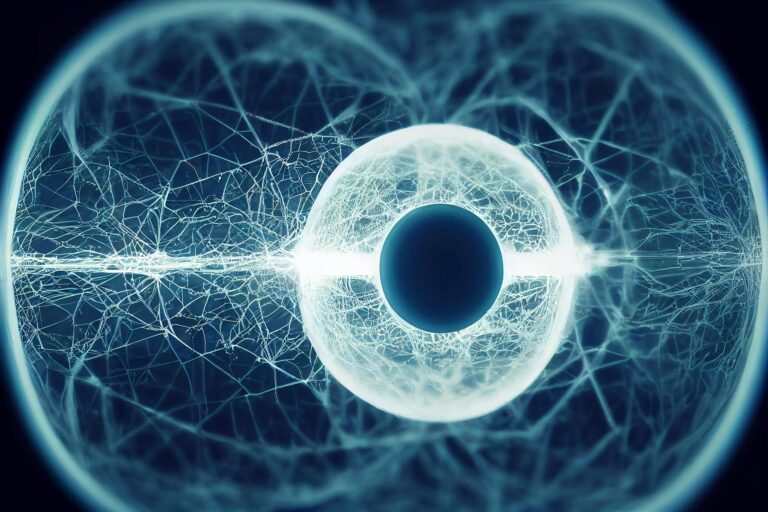
Research continues to push the boundaries of how early and how accurately amyloid pathology can be detected. Beyond the blood tests currently entering clinical practice, scientists are exploring retinal imaging as a window into brain amyloid status. The retina, as an extension of the central nervous system, may harbor detectable amyloid deposits that mirror those in the brain. If validated, a simple eye exam could one day flag individuals for more detailed evaluation.
Digital biomarkers represent another promising frontier. Subtle changes in speech patterns, typing rhythms, and even smartphone usage may precede obvious cognitive symptoms by years. Machine learning algorithms trained on these behavioral signals could identify at-risk individuals through passive monitoring, prompting proactive medical evaluation. While these technologies remain investigational, they suggest a future where early detection becomes seamlessly integrated into daily life rather than requiring specialized medical procedures.
How to Prepare
- **Document your cognitive baseline.** Before any testing, create a record of your current cognitive function using validated self-assessment tools or formal neuropsychological testing. This baseline becomes invaluable for tracking changes over time, regardless of amyloid status.
- **Research your family history thoroughly.** Gather detailed information about relatives who developed dementia, including age of onset, progression pattern, and any autopsy results if available. First-degree relatives with early-onset Alzheimer’s significantly increase your statistical risk.
- **Identify appropriate specialists in your area.** Search for neurologists with expertise in cognitive disorders or memory clinics affiliated with academic medical centers. These specialists have the most experience interpreting biomarker results and discussing treatment options.
- **Understand your insurance coverage and financial options.** Contact your insurance provider directly to clarify coverage for PET scans, CSF analysis, and blood-based biomarkers. Explore clinical trial databases for studies that include diagnostic testing.
- **Consider genetic testing for APOE status.** Knowing whether you carry the APOE4 allele provides context for interpreting amyloid results and may influence treatment decisions. Genetic counseling before and after testing helps manage the emotional dimensions of this information.
How to Apply This
- **Schedule an initial consultation with your primary care physician.** Present your concerns, family history documentation, and desire to pursue biomarker testing. Request referral to a cognitive specialist if your physician lacks experience with these assessments.
- **Undergo comprehensive cognitive evaluation.** Complete neuropsychological testing to establish objective measures of memory, executive function, language, and other domains. These results help interpret biomarker findings in clinical context.
- **Proceed with biomarker testing appropriate to your situation.** Work with specialists to determine whether blood tests, CSF analysis, PET imaging, or some combination best suits your needs, symptoms, and risk profile.
- **Develop a monitoring and action plan based on results.** Whether positive or negative, create a schedule for follow-up testing, lifestyle interventions, and criteria for considering treatment. Document this plan and share it with family members or healthcare proxies.
Expert Tips
- **Request copies of all imaging and laboratory results.** Maintaining personal records enables second opinions and ensures continuity if you change healthcare providers or relocate.
- **Join a research registry even if you do not qualify for current trials.** Organizations like the Alzheimer’s Prevention Registry connect participants with emerging studies and contribute to scientific progress regardless of individual eligibility.
- **Address modifiable risk factors regardless of amyloid status.** Cardiovascular health, sleep quality, hearing loss, and social engagement all influence cognitive outcomes and remain within your control.
- **Establish legal and financial documents while cognitively healthy.** Advance directives, powers of attorney, and long-term care preferences should be formalized before any impairment develops.
- **Connect with support organizations proactively.** The Alzheimer’s Association and similar groups offer resources for individuals at every stage, including those recently diagnosed and those simply concerned about their risk.
Conclusion
The capacity to detect amyloid accumulation years or decades before dementia develops represents a genuine paradigm shift in Alzheimer’s care. This early window creates opportunities that simply did not exist a generation ago””opportunities to intervene with disease-modifying treatments, to participate in research advancing the field, and to make informed decisions about the future with clarity rather than uncertainty. The science is not yet perfected, the treatments not yet ideal, but the trajectory points unmistakably toward earlier detection and earlier intervention as the path forward.
For individuals navigating these decisions, the key lies in balancing proactive engagement with realistic expectations. Early amyloid detection does not guarantee prevention of dementia, nor does a negative result ensure permanent cognitive health. What testing provides is information””information that enables planning, informs treatment discussions, and replaces vague worry with concrete data. That knowledge, wielded thoughtfully in partnership with skilled clinicians, offers the best current approach to protecting brain health across the lifespan.
Frequently Asked Questions
How long does it typically take to see results?
Results vary depending on individual circumstances, but most people begin to see meaningful progress within 4-8 weeks of consistent effort. Patience and persistence are key factors in achieving lasting outcomes.
Is this approach suitable for beginners?
Yes, this approach works well for beginners when implemented gradually. Starting with the fundamentals and building up over time leads to better long-term results than trying to do everything at once.
What are the most common mistakes to avoid?
The most common mistakes include rushing the process, skipping foundational steps, and failing to track progress. Taking a methodical approach and learning from both successes and setbacks leads to better outcomes.
How can I measure my progress effectively?
Set specific, measurable goals at the outset and track relevant metrics regularly. Keep a journal or log to document your journey, and periodically review your progress against your initial objectives.
When should I seek professional help?
Consider consulting a professional if you encounter persistent challenges, need specialized expertise, or want to accelerate your progress. Professional guidance can provide valuable insights and help you avoid costly mistakes.
What resources do you recommend for further learning?
Look for reputable sources in the field, including industry publications, expert blogs, and educational courses. Joining communities of practitioners can also provide valuable peer support and knowledge sharing.