Elderly people tend to experience more frequent foot cramps due to a combination of physiological changes, health conditions, and lifestyle factors that affect muscle function, blood flow, and nerve health as they age.
One major reason is **reduced blood circulation** to the feet and lower legs. As people get older, their blood vessels can become narrower and less flexible due to conditions like peripheral artery disease and atherosclerosis. This narrowing limits the amount of oxygen and nutrients reaching the muscles, which can cause muscles to cramp more easily, especially during activity or at rest. Poor circulation also slows healing and can cause muscles to weaken over time, increasing cramp risk. Additionally, the skin and tissues in the feet become thinner and drier, making the feet more vulnerable to injury and discomfort that can trigger cramps.
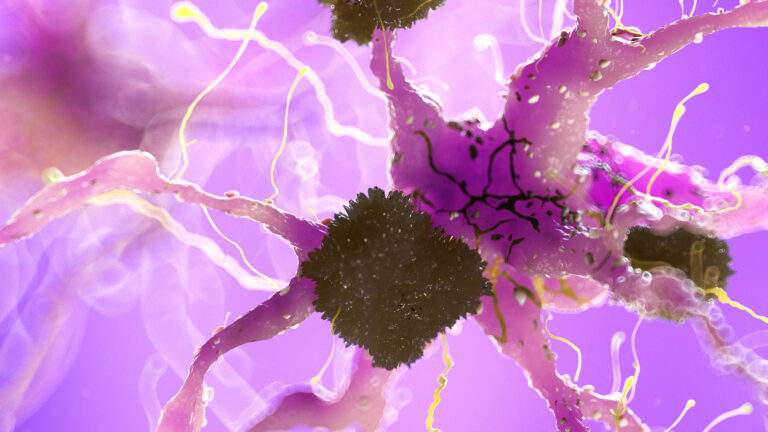
Another important factor is **muscle and nerve changes** that occur with aging. Muscle mass and strength naturally decline, a process called sarcopenia, which can lead to muscle fatigue and spasms. Nerve function also deteriorates with age, sometimes causing compression or irritation of nerves that control the feet muscles. This nerve involvement can provoke involuntary muscle contractions or cramps. Conditions such as pinched nerves in the spine or neuropathy (nerve damage often related to diabetes or other diseases) are more common in older adults and contribute to cramping.
**Electrolyte imbalances** are also more frequent in elderly individuals. Minerals like potassium, calcium, and magnesium are essential for proper muscle contraction and relaxation. Aging, combined with medications (such as diuretics for blood pressure), dehydration, or poor diet, can lead to deficiencies in these electrolytes, making muscles more prone to cramping.
Furthermore, **fat pad atrophy** in the feet reduces natural cushioning under the heels and balls of the feet. This loss of padding increases pressure and discomfort during walking or standing, which can cause muscle strain and cramps. Dry, cracked skin and swelling from fluid retention or other medical conditions can also exacerbate discomfort and muscle spasms.
Lifestyle factors common in older adults, such as **reduced physical activity**, prolonged sitting or standing, and inadequate stretching, contribute to tight calf muscles and poor muscle conditioning, which are known to increase cramp frequency. Inactivity leads to muscle stiffness and weakness, making cramps more likely.
Certain **medical conditions** prevalent in the elderly, including diabetes, kidney disease, thyroid disorders, and vascular diseases, can cause or worsen muscle cramps. Medications used to treat these conditions may also have side effects that promote cramping.
In summary, the increased frequency of foot cramps in elderly people is due to a complex interplay of reduced blood flow, muscle and nerve degeneration, electrolyte imbalances, loss of foot cushioning, and lifestyle or medical factors that impair muscle health and function. These elements combine to make the muscles in the feet more susceptible to painful, involuntary contractions.