Dementia, a progressive neurological disorder, affects millions of people worldwide, causing a decline in cognitive function and memory loss. As dementia progresses, it can severely impair an individual’s ability to perform daily activities. One of the critical factors in understanding dementia is the role of brain structures, particularly white and gray matter. In this article, we will discuss the differences between white and gray matter, their functions in the brain, and how they relate to dementia.
Understanding White and Gray Matter
White matter and gray matter are the two primary components of the central nervous system, and they serve different functions within the brain.
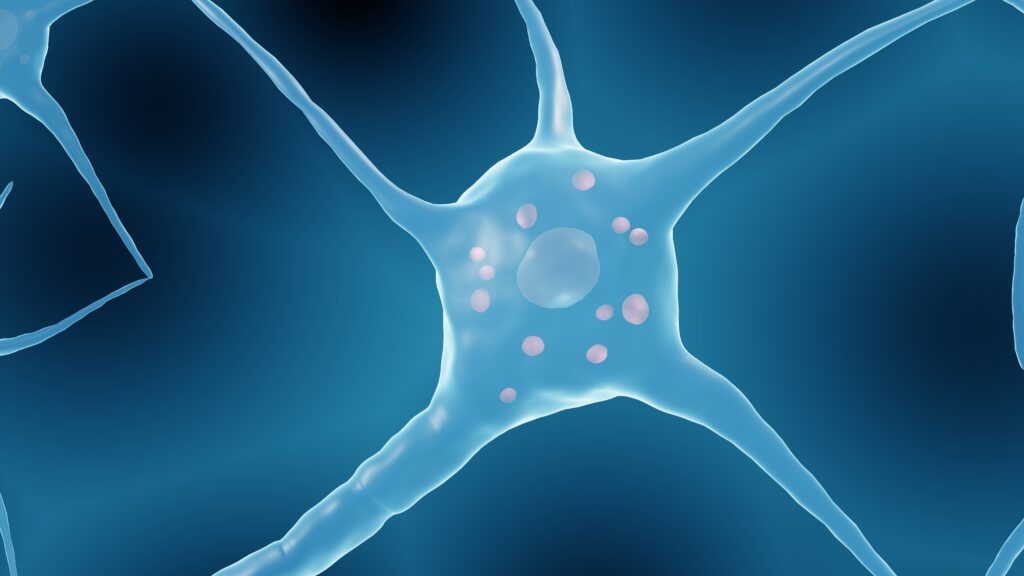
- Gray Matter: The gray matter consists of neuronal cell bodies, dendrites, and synapses, which are essential for processing and transmitting information within the brain. It is responsible for various cognitive functions, including memory, language, and decision-making. Gray matter is found in the outer layers of the brain (cortex) and deeper regions such as the hippocampus, which plays a crucial role in memory formation.
- White Matter: White matter, on the other hand, consists of myelinated axons, which are nerve fibers coated with a fatty substance called myelin. Myelin insulates the axons, allowing for faster and more efficient transmission of electrical signals between different brain regions. White matter acts as the brain’s communication network, connecting different gray matter regions and enabling them to work together.
The Relationship Between White Matter, Gray Matter, and Dementia
Research has found that both white and gray matter are affected in dementia, but the extent of their involvement and their specific roles in disease progression can vary depending on the type of dementia.
- Alzheimer’s Disease: Alzheimer’s disease is the most common form of dementia, accounting for approximately 60-80% of cases. It is characterized by the presence of amyloid plaques and neurofibrillary tangles in the brain, which lead to the loss of neurons and synapses, primarily in the gray matter. This loss results in the atrophy of gray matter areas, such as the hippocampus and the cortex, which are crucial for memory and cognition. White matter is also affected in Alzheimer’s disease, with studies showing a reduction in white matter integrity and connectivity, which can contribute to cognitive decline.
- Vascular Dementia: Vascular dementia, the second most common form of dementia, results from reduced blood flow to the brain due to damaged blood vessels. This lack of blood flow can cause damage to both white and gray matter. In vascular dementia, white matter is often more severely affected, with small vessel disease causing white matter lesions, leading to disrupted communication between brain regions and cognitive decline.
- Frontotemporal Dementia: Frontotemporal dementia is a less common form of dementia characterized by the degeneration of the frontal and temporal lobes. Gray matter atrophy is a significant feature of this condition, specifically in the affected brain regions. However, white matter degeneration can also occur, disrupting the neural networks between the frontal and temporal lobes and contributing to the progressive decline in cognitive and behavioral functions.
Understanding the roles and differences between white and gray matter is essential for comprehending the complex nature of dementia. While both white and gray matter are affected in various types of dementia, the specific involvement of these brain components depends on the underlying disease process. Future research focusing on the interaction between white and gray matter and the development of targeted therapies can potentially lead to more effective treatments for dementia, improving the quality of life for millions of people worldwide.