Meningitis in adults is caused by inflammation of the protective membranes covering the brain and spinal cord, known as the meninges. This inflammation can be triggered by various infectious agents including bacteria, viruses, fungi, parasites, and rarely amoebas. The specific cause influences how meningitis develops, how severe it becomes, and what treatments are necessary.
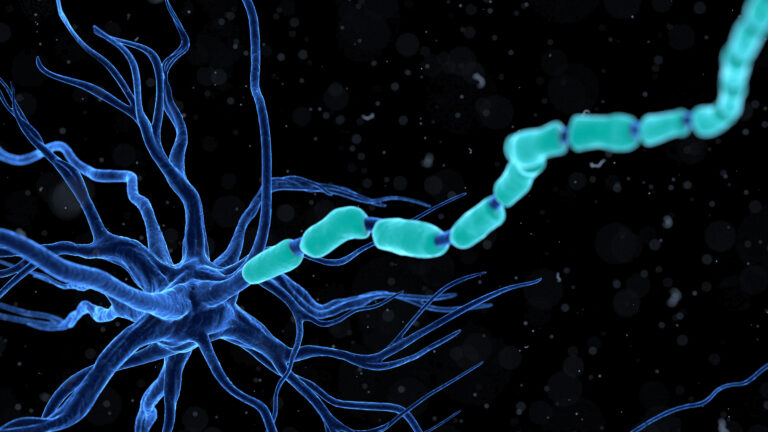
**Bacterial Meningitis** is one of the most serious forms affecting adults. It occurs when bacteria invade the meninges and multiply rapidly. Common bacterial culprits include *Streptococcus pneumoniae*, which is the most frequent cause in adults; *Neisseria meningitidis* (meningococcal bacteria), which can spread quickly especially in close living quarters; *Haemophilus influenzae* type b (Hib); and sometimes *Staphylococcus aureus*, particularly after head trauma or neurosurgical procedures. These bacteria often live harmlessly in people’s noses or throats but can become dangerous if they enter the bloodstream or directly infect the meninges through wounds or other routes.
Bacterial meningitis spreads primarily through respiratory droplets from coughing, sneezing, kissing, or sharing utensils with an infected person. However, not everyone exposed will develop disease because a healthy immune system may prevent infection from progressing to meningitis. When it does occur though, bacterial meningitis causes symptoms such as sudden high fever, severe headache that doesn’t go away with usual remedies, neck stiffness making it hard to touch chin to chest without pain or resistance, nausea and vomiting without clear reason, sensitivity to light (photophobia), confusion or difficulty waking up—all signs that require immediate medical attention.
**Viral Meningitis**, on the other hand, tends to be more common but usually less severe than bacterial forms. Many different viruses can cause this condition—enteroviruses are among the most frequent offenders—but others include herpes simplex virus and mumps virus among many others worldwide depending on seasonality and geography. Viral infections reach the central nervous system typically via blood circulation after initial infection elsewhere like respiratory tract or gastrointestinal system. Symptoms overlap with bacterial cases but often improve within a week without specific antiviral treatment except for some exceptions like herpesvirus infections.
**Fungal Meningitis** is much rarer in healthy adults but occurs mainly in those with weakened immune systems such as HIV/AIDS patients or those on immunosuppressive drugs following organ transplants. Fungi like *Cryptococcus neoformans* enter through inhalation into lungs first then disseminate into bloodstream reaching brain coverings causing chronic inflammation that develops slowly over weeks rather than hours.
**Parasitic Meningitis**, caused by certain parasites invading nervous tissue either directly through contaminated food/water sources or via insect vectors transmitting larvae stages inside humans also exists but remains uncommon overall compared to viral/bacterial causes.
A very rare form called **Amebic Meningitis**, caused by free-living amoebas found mostly in warm freshwater environments entering nasal passages during swimming activities leads to rapid fatal brain infection despite aggressive treatment attempts.
In summary of causative factors:
– **Bacteria:** Most dangerous; spread via close contact respiratory secretions; examples include pneumococcus (*Streptococcus pneumoniae*), meningococcus (*Neisseria meningitidis*), Hib.
– **Viruses:** More common but milder; transmitted through various routes depending on virus type.
– **Fungi:** Affect immunocompromised individuals mainly.
– **Parasites & Amoebas:** Rare causes linked mostly to environmental exposures.
Understanding these causes helps guide prevention strategies such as vaccination against key bacteria strains (meningococcal vaccine for *N.meningitidis*, pneumococcal vaccine for *S.pneumoniae*, Hib vaccine), practicing good hygiene like handwashing and avoiding sharing utensils during illness periods especially where outbreaks occur.
When symptoms suggestive of meningitis appear—f