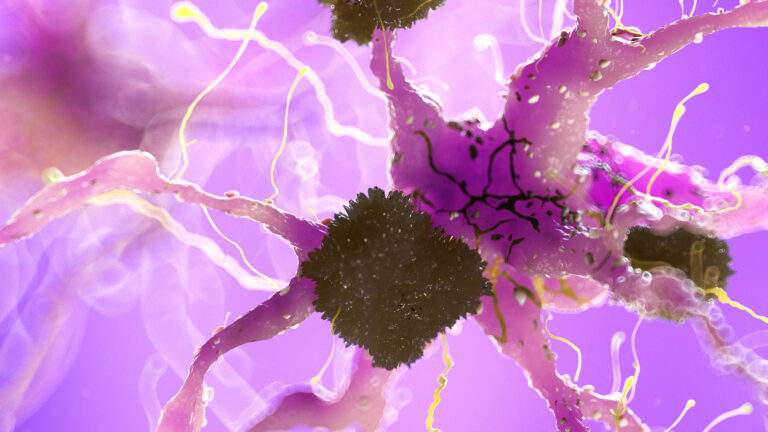
Resting state functional magnetic resonance imaging (resting state fMRI or rs-fMRI) studies in dementia explore how the brain functions when a person is not performing any specific task, essentially capturing the brain’s activity at rest. This technique measures spontaneous fluctuations in blood oxygen levels across different brain regions, which reflect neural activity and connectivity patterns. These patterns are crucial because they reveal how different parts of the brain communicate and coordinate with each other, even when the brain is “idle.” In dementia research, resting state fMRI is particularly valuable because it helps identify disruptions in brain networks that are associated with cognitive decline and neurodegenerative diseases.
Dementia, including Alzheimer’s disease and other related disorders, involves progressive deterioration of memory, thinking, and behavior. Traditional imaging techniques often focus on structural changes in the brain, such as shrinkage or lesions. However, resting state fMRI provides a window into the brain’s functional organization, showing how networks of neurons interact dynamically. This is important because dementia affects not only the physical structure of the brain but also the way brain regions communicate, which can precede visible structural damage.
One of the key concepts in resting state fMRI is the identification of intrinsic brain networks. The most studied network in dementia is the Default Mode Network (DMN), which includes regions like the medial prefrontal cortex, posterior cingulate cortex, and lateral parietal cortex. The DMN is active when a person is at rest and not focused on the outside world, involved in self-referential thinking and memory retrieval. In dementia, especially Alzheimer’s disease, the DMN shows reduced connectivity and altered activity patterns. This disruption correlates with memory loss and cognitive impairment, making it a biomarker for early detection and progression monitoring.
Resting state fMRI studies in dementia typically involve scanning patients while they lie still with their eyes open or closed, without engaging in any task. The resulting data undergo complex processing to remove noise and artifacts, such as head movement or physiological signals like heartbeat and breathing. After preprocessing, researchers analyze the temporal correlations between different brain regions to map functional connectivity. Changes in these connectivity patterns can indicate the presence and severity of dementia.
Beyond the DMN, other brain networks are also studied in dementia using resting state fMRI. These include the Salience Network, which helps detect and filter important stimuli; the Executive Control Network, involved in decision-making and attention; and sensory-motor networks. Alterations in these networks can explain various symptoms of dementia, such as difficulties in attention, problem-solving, and motor function.
Resting state fMRI is also used to differentiate between types of dementia. For example, vascular dementia, Lewy body dementia, and frontotemporal dementia each show distinct patterns of network disruption. This helps clinicians improve diagnosis accuracy and tailor treatments. Moreover, resting state fMRI can track disease progression and response to interventions by monitoring changes in brain connectivity over time.
One of the exciting developments in this field is the integration of resting state fMRI data with artificial intelligence and machine learning techniques. These approaches analyze large datasets to identify subtle patterns that may not be visible to human observers. AI models can predict disease progression, classify dementia stages, and even forecast cognitive decline with high accuracy. This enhances the potential of resting state fMRI as a tool for early diagnosis and personalized medicine.
Despite its promise, resting state fMRI in dementia research faces challenges. The brain’s resting activity is inherently variable, and factors like age, medication, and comorbidities can influence results. Standardizing data acquisition and analysis protocols is essential to ensure reproducibility and comparability across studies. Additionally, interpreting functional connectivity changes requires careful consideration, as decreased or increased connectivity can have different implications depending on the brain region and disease stage.
In summary, resting state fMRI studies in dementia provide a powerful method to understand how brain networks are altered in neurodegenerative diseases. By revealing changes in functional connectivity, these studies offer insights into the mechanisms underlying cognitive decline an