Understanding the Connection Between Acetylcholine and Dementia: Insights and Implications
Dementia is a syndrome that affects memory, cognition, behavior, and the ability to perform everyday activities, with Alzheimer’s disease (AD) as its most common cause. Researchers have long been fascinated by the complexities of the human brain and the biochemical processes that underpin dementia, specifically focusing on neurotransmitters, the chemical messengers of the nervous system. One such neurotransmitter, acetylcholine, has been a subject of particular interest due to its critical role in memory and cognition. Evidence shows a significant link between decreased acetylcholine levels and the onset of dementia, especially Alzheimer’s disease.
The Role of Acetylcholine
Acetylcholine, discovered in the early 20th century, is a neurotransmitter produced in the neurons of the brain and peripheral nervous system. It has many roles, but its most pertinent function in the context of dementia is facilitating synaptic transmission in the brain’s cholinergic system, the nerve cells that use acetylcholine to send messages. The cholinergic system is involved in numerous cognitive processes, including attention, learning, and memory. Disruptions to this system are believed to contribute significantly to the cognitive impairments seen in dementia.
Acetylcholine and Dementia: The Connection
The association between acetylcholine levels and dementia is based on the ‘cholinergic hypothesis,’ which postulates that Alzheimer’s disease is primarily caused by reduced synthesis of the neurotransmitter acetylcholine. The hypothesis was suggested in the late 1970s when researchers observed a loss of cholinergic neurons in the brains of individuals with Alzheimer’s.
These observations have since been corroborated by numerous studies, which have consistently demonstrated that the density of cholinergic neurons decreases significantly in the brains of Alzheimer’s patients, leading to reduced acetylcholine levels. This deficiency affects the cholinergic pathways associated with cognitive processes such as memory and attention, thereby contributing to the cognitive decline characteristic of dementia.
Notably, this decline in acetylcholine levels is not uniform across the brain. The most significant decreases are observed in the cerebral cortex and the hippocampus, areas critical for memory and cognition. The selective vulnerability of these regions may explain the particular cognitive deficits seen in Alzheimer’s disease and other forms of dementia.
Implications for Treatment
Understanding the link between acetylcholine and dementia has significant implications for therapeutic interventions. The cholinergic hypothesis has been a guiding principle in the development of treatments for Alzheimer’s disease and other dementias.
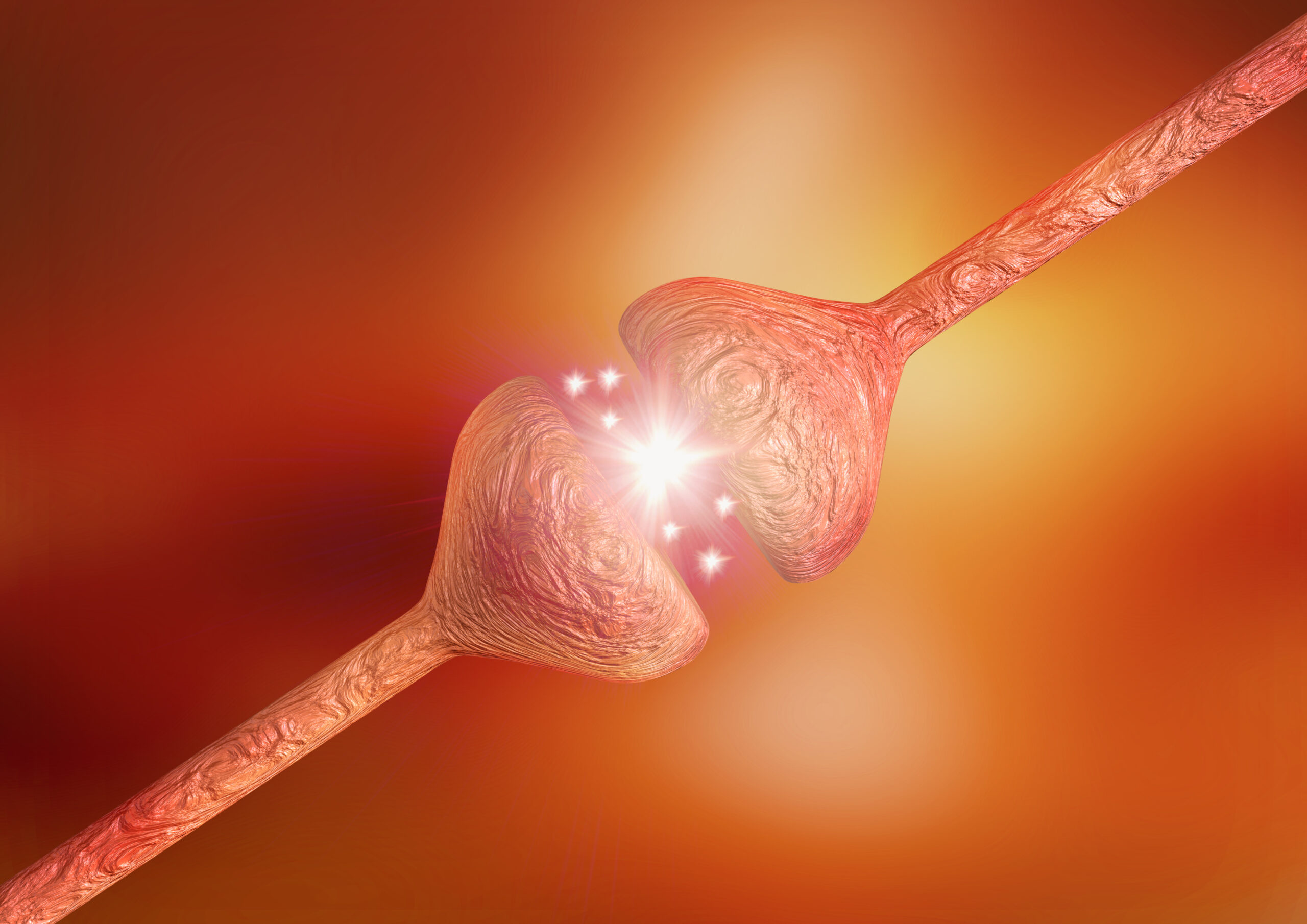
Cholinesterase inhibitors are a class of drugs that were developed based on this understanding. These medications work by blocking the enzyme acetylcholinesterase, which breaks down acetylcholine in the synaptic cleft. By inhibiting this enzyme, these drugs increase the amount of acetylcholine available for transmission, thereby enhancing communication between neurons and potentially improving cognitive function.
Donepezil, rivastigmine, and galantamine are examples of cholinesterase inhibitors that have been approved for the treatment of mild to moderate Alzheimer’s disease. While these drugs cannot reverse the progression of Alzheimer’s, they can temporarily slow down the worsening of symptoms and improve quality of life for some patients.
Limitations and Future Research Directions
Despite the established link between acetylcholine and dementia, it is important to note that the cholinergic hypothesis does not fully explain the pathogenesis of Alzheimer’s disease or other dementias. Alzheimer’s, in particular, is now understood to be a multifactorial disease, with other pathological features such as beta-amyloid plaques and tau tangles playing crucial roles. Moreover, cholinesterase inhibitors are not universally effective and do not stop the disease’s progression, indicating that other mechanisms are at work.
In addition, the relationship between acetylcholine and dementia is not unidirectional. While reduced acetylcholine levels may contribute to cognitive decline, the reverse can also occur: the neurodegenerative processes of dementia can lead to a decrease in acetylcholine production. This complex interplay suggests a vicious cycle wherein cognitive decline and acetylcholine deficiency exacerbate one another.
Nonetheless, the exploration of the acetylcholine-dementia link has led to advancements in our understanding of dementia’s neurochemical basis and spurred the development of potential therapeutic strategies. Future research could focus on augmenting existing cholinergic treatments with other approaches that target the myriad factors contributing to dementia.
The study of the cholinergic system’s role in cognitive decline is still ongoing. Neuroimaging techniques are being used to visualize the loss of cholinergic neurons in living patients, enhancing our understanding of how the cholinergic system changes over the course of dementia.
Also, scientists are studying other aspects of the cholinergic system, such as the role of acetylcholine receptors. There are two main types of acetylcholine receptors in the brain – nicotinic and muscarinic – and both types are involved in cognitive processes. There is evidence to suggest that dysfunction in these receptors may also contribute to dementia, and targeting these receptors could be a novel approach to treatment.
Moreover, considering the multifactorial nature of Alzheimer’s disease, researchers are exploring combination therapies that not only enhance acetylcholine levels but also target other pathological features, such as beta-amyloid plaques and tau tangles. There is also a growing interest in lifestyle factors that could influence the cholinergic system, such as diet, exercise, and sleep, which could potentially be harnessed for prevention or treatment strategies.
Our understanding of the link between acetylcholine and dementia has grown tremendously over the years, illuminating the role of this crucial neurotransmitter in cognitive function and dysfunction. While the relationship between acetylcholine and dementia is complex and not fully understood, this line of research has led to the development of important therapeutic strategies and continues to inspire novel approaches to dementia treatment and prevention. As we delve further into the intricacies of the cholinergic system and its interaction with other factors contributing to dementia, we move closer to more effective strategies for managing this debilitating syndrome.