Medicaid Work Requirements: Smart Reform or Unfair Burden?
In recent years, the idea of implementing work requirements for Medicaid recipients has been a topic of heated debate. This concept, which gained significant attention during Donald Trump’s presidency, aims to condition Medicaid coverage on certain activities like working, volunteering, or attending school. Proponents argue that such requirements promote self-sufficiency and employment, while critics see them as an unfair burden on vulnerable populations.
### Background on Medicaid Work Requirements
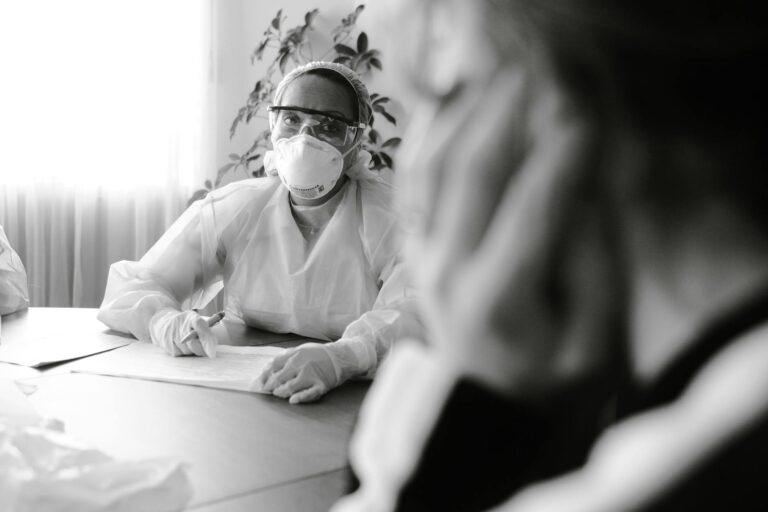
Medicaid is a state-federal health insurance program designed for low-income individuals and families. During Trump’s first administration, the Centers for Medicare and Medicaid Services (CMS) encouraged states to apply for Section 1115 waivers, which allowed them to impose work requirements as a condition for Medicaid eligibility. Thirteen states received approval for these waivers, but only Arkansas implemented them with consequences for noncompliance, resulting in over 18,000 people losing coverage[1][4].
### The Debate
Supporters of work requirements argue that they incentivize employment and reduce dependency on welfare. However, research suggests that most Medicaid recipients are already working or face significant barriers to employment, such as caregiving responsibilities or disabilities[1][5]. The Congressional Budget Office (CBO) has estimated that implementing national work requirements would lead to significant coverage losses without increasing employment rates[1][4].
### Impact on Vulnerable Groups
Critics argue that work requirements disproportionately harm disadvantaged groups, including people with disabilities, women, and those in low-wage jobs. The experience in Arkansas showed that many individuals lost coverage not because they failed to meet work requirements, but due to difficulties with the reporting system[5]. This can lead to severe consequences, such as delayed medical care and increased medical debt[5].
### Current Developments
Despite these challenges, some states are revisiting work requirements. Georgia, the only state currently enforcing such requirements, is proposing changes to simplify the program by removing monthly reporting and premium payments[3]. Arkansas is also seeking to revive its program with a new approach that uses data to assess compliance rather than requiring enrollees to report their work hours[3].
### Conclusion
The debate over Medicaid work requirements highlights a broader discussion about the role of welfare programs in society. While proponents see these requirements as a way to promote self-sufficiency, critics argue that they overlook the complex realities faced by low-income individuals and can lead to unintended consequences like reduced health coverage. As policymakers continue to consider these requirements, it is crucial to weigh the potential benefits against the potential harm to vulnerable populations.