Cerebral palsy (CP) is a complex neurological disorder primarily characterized by impaired movement and posture, resulting from non-progressive brain injury or malformation occurring during the developing fetal or infant brain. One important area of investigation is whether **maternal infections that are untreated or inadequately treated during pregnancy contribute to the risk of cerebral palsy** in the child.
**Maternal infections and inflammation during pregnancy are strongly linked to brain injury mechanisms that can lead to cerebral palsy.** A key example is chorioamnionitis, an infection and inflammation of the fetal membranes (chorion and amnion) and placenta. This condition triggers a robust inflammatory response involving maternal and fetal immune cells such as neutrophils, monocytes, and macrophages, which release cytokines and chemokines. These inflammatory mediators can cross the placental barrier and induce neuroinflammation in the developing fetal brain, disrupting critical processes like myelin formation and neuronal development[1].
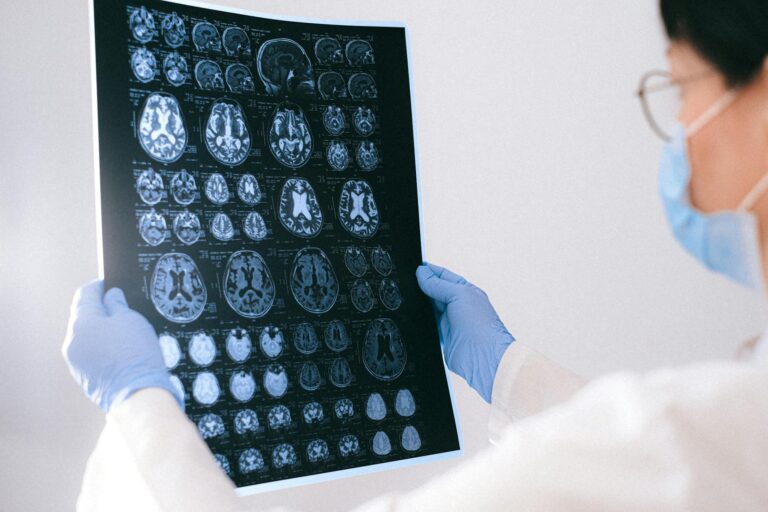
The placenta acts as a critical interface where maternal infections can influence fetal brain health. Inflammation in the placenta, often due to untreated infections, can impair oxygen and nutrient delivery and promote neuroinflammatory cascades that damage the fetal brain. This damage can manifest as white matter injury, a common neuropathological substrate of cerebral palsy[1].
**Epidemiological and clinical studies support the association between maternal infections and increased cerebral palsy risk.** For example, histologic chorioamnionitis has been linked to adverse neurodevelopmental outcomes, including cerebral palsy, especially in preterm infants. However, the relationship is complex: some studies suggest that mild or early-stage chorioamnionitis might paradoxically reduce CP risk, while severe or advanced inflammation increases it[4][5]. This indicates that the timing, severity, and management of infection and inflammation are critical factors.
**Failure to treat maternal infections effectively may exacerbate these risks.** Untreated infections allow prolonged inflammation, increasing fetal exposure to damaging cytokines and immune cells. This can lead to hypoxic-ischemic injury (oxygen deprivation), which is another major pathway to cerebral palsy. For instance, neonatal acidemia (low blood pH due to oxygen deprivation) at birth, which can result from placental inflammation and infection, is strongly associated with higher risks of cerebral palsy and other neurodevelopmental disorders[2].
**Preventing and managing maternal infections during pregnancy is therefore a crucial strategy to reduce cerebral palsy incidence.** Early diagnosis and treatment of infections such as bacterial vaginosis, urinary tract infections, and chorioamnionitis can reduce placental inflammation and fetal brain injury. Research continues to explore novel targets to reduce preterm birth and inflammation-related neonatal brain injury, which are important contributors to cerebral palsy[3].
In summary, **there is authoritative evidence that untreated or inadequately treated maternal infections contribute to inflammatory processes in the placenta and fetal brain that increase the risk of cerebral palsy.** The exact risk depends on the infection type, timing, severity, and treatment. Effective prenatal care that includes screening and treating infections is essential to mitigate this risk.
—
**Sources:**
[1] The placenta as a window into neonatal brain injury – PMC, https://pmc.ncbi.nlm.nih.gov/articles/PMC12448110/
[2] Umbilical cord acidemia linked to long-term neurodevelopmental risk