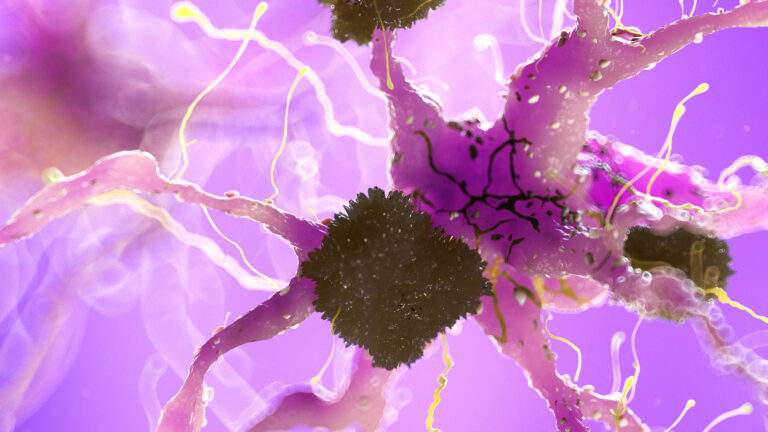
Magnetic Resonance Imaging (MRI) is a powerful tool that helps doctors and researchers see inside the brain without surgery. When it comes to dementia, a condition where brain function declines over time, MRI plays a crucial role in revealing how brain connectivity—the way different parts of the brain communicate—is lost. Understanding this connectivity loss is essential because dementia, including Alzheimer’s disease, is not just about brain cells dying but also about how the brain’s networks break down.
At its core, MRI uses strong magnetic fields and radio waves to create detailed images of the brain’s structure and function. There are different types of MRI scans, but two are especially important for studying dementia: structural MRI and functional MRI (fMRI). Structural MRI shows the physical anatomy of the brain, such as the size and shape of different regions, while fMRI measures brain activity by detecting changes in blood flow, which reflects how brain regions communicate during rest or tasks.
In dementia patients, structural MRI often reveals shrinkage or atrophy in specific brain areas. For example, the hippocampus, a region critical for memory, tends to shrink early in Alzheimer’s disease. This shrinkage indicates loss of neurons and connections. However, structural changes alone don’t tell the whole story. The brain is a complex network, and how different parts connect and work together is just as important as their size.
This is where functional MRI becomes invaluable. fMRI can detect changes in brain connectivity by measuring how different regions activate in sync. In healthy brains, certain networks, like the default mode network (DMN), show strong connectivity, meaning these areas communicate efficiently. In dementia, studies have shown that this connectivity weakens, especially in networks involving the frontal and temporal lobes, which are vital for memory, language, and executive functions.
Loss of connectivity means that even if some brain cells remain, their ability to send and receive signals is impaired. This disruption can explain many symptoms of dementia, such as memory loss, confusion, and difficulty with problem-solving. For example, reduced frontotemporal connectivity has been linked to worse cognitive performance in Alzheimer’s patients.
MRI can also detect subtle changes before symptoms become obvious. Alterations in MRI-visible perivascular spaces—small fluid-filled spaces around blood vessels in the brain—have been observed years before dementia diagnosis. These changes may reflect early vascular or clearance problems that contribute to connectivity loss and brain damage over time.
Advanced MRI techniques can map the brain’s white matter tracts, the “wiring” that connects different brain regions. Diffusion tensor imaging (DTI), a type of MRI, tracks the movement of water molecules along these tracts. In dementia, DTI often shows reduced integrity of white matter pathways, indicating that the brain’s communication highways are breaking down. This loss of white matter integrity correlates with cognitive decline and helps differentiate between normal aging and dementia.
Moreover, MRI can reveal amyloid-related imaging abnormalities (ARIA), which are changes in the brain related to amyloid protein buildup—a hallmark of Alzheimer’s disease. Monitoring these abnormalities is important, especially in patients receiving treatments targeting amyloid, as MRI can detect brain swelling or fluid buildup that might signal side effects or disease progression.
In summary, MRI reveals connectivity loss in dementia patients by showing both structural damage and functional disconnection in the brain. It highlights shrinking brain regions, disrupted communication networks, deteriorating white matter tracts, and early vascular changes. This comprehensive view helps clinicians understand the disease’s progression, differentiate dementia types, monitor treatment effects, and potentially identify the condition earlier than clinical symptoms alone would allow. Through these insights, MRI continues to be an indispensable tool in unraveling the complex brain changes underlying dementia.