Gut health plays a crucial role in dementia prevention through its complex and dynamic relationship with the brain, often referred to as the gut-brain axis. This connection involves multiple pathways by which the state of the gut microbiome—the trillions of microorganisms living in the digestive tract—can influence brain health, cognitive function, and the risk of neurodegenerative diseases like dementia.
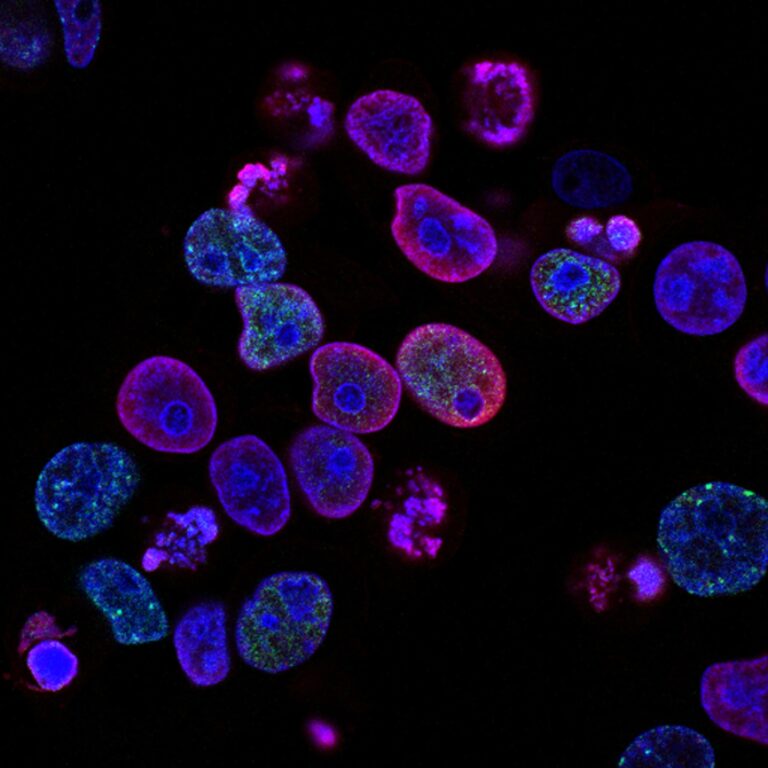
The gut microbiome affects dementia risk primarily by modulating inflammation, immune responses, and the production of key metabolites that impact brain function. When the gut microbiota is balanced and diverse, it produces beneficial compounds such as short-chain fatty acids (SCFAs) that support the integrity of the gut lining and reduce systemic inflammation. This, in turn, helps maintain the blood-brain barrier, a critical shield protecting the brain from harmful substances. Conversely, an imbalanced gut microbiome, or dysbiosis, can lead to increased gut permeability (“leaky gut”), allowing inflammatory molecules and toxins to enter the bloodstream and eventually reach the brain, promoting neuroinflammation—a key driver of dementia pathology.
One important mechanism linking gut health to dementia involves the vagus nerve, which provides a direct communication highway between the gut and the brain. Signals transmitted via the vagus nerve can influence brain inflammation and neurotransmitter balance, affecting cognition and mood. Disruptions in this gut-brain communication have been associated with increased accumulation of amyloid-beta plaques and tau protein tangles, hallmark features of Alzheimer’s disease, the most common form of dementia.
Diet is a major factor shaping the gut microbiome and thus influencing dementia risk. Diets rich in fiber, plant-based foods, and healthy fats—such as the Mediterranean diet—promote a healthy gut microbiota composition. This diet increases the production of anti-inflammatory metabolites and supports brain-protective pathways. Studies have shown that adherence to such diets can modulate metabolites linked to dementia risk, especially in individuals genetically predisposed to Alzheimer’s disease, such as those carrying the APOE4 gene variant.
Emerging therapeutic approaches targeting the gut microbiome show promise in dementia prevention and treatment. Probiotics and prebiotics can help restore microbial balance, reduce inflammation, and improve cognitive function. More experimental interventions like fecal microbiota transplantation (FMT) have demonstrated the ability to remodel the gut ecosystem, reduce amyloid-beta burden, and reverse pathological brain changes in animal models, suggesting potential future applications in humans.
Beyond diet and microbiota-targeted therapies, gut health also intersects with other systemic factors influencing dementia risk. For example, gastrointestinal disorders such as irritable bowel syndrome (IBS) and nutrient deficiencies like low vitamin D levels have been linked to higher risks of Alzheimer’s and Parkinson’s diseases. Metabolic conditions like type 2 diabetes, which affect both gut and brain health, further illustrate the interconnectedness of these systems.
In summary, maintaining a healthy gut microbiome through balanced nutrition, lifestyle, and potentially microbiota-based therapies can reduce neuroinflammation, support brain barrier integrity, and modulate metabolic and immune pathways that collectively lower the risk of dementia. The gut-brain axis represents a vital frontier in understanding and preventing cognitive decline, highlighting the importance of gut health as a foundational pillar for brain longevity.