Cerebral palsy (CP) profoundly affects reflexes due to its impact on the brain areas responsible for motor control and muscle coordination. Reflexes are automatic, involuntary responses to stimuli, and in CP, these reflexes can be abnormal—either exaggerated, diminished, or persistently present beyond the typical developmental period.
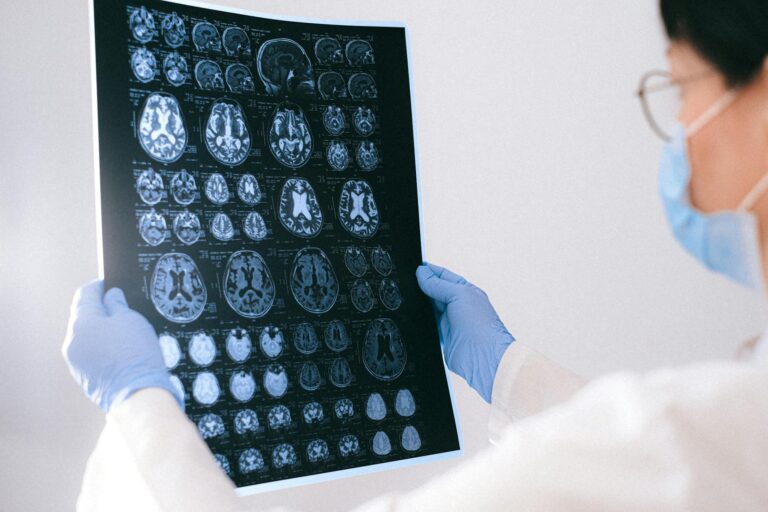
In children with CP, damage or abnormal development in the brain, particularly in the motor cortex, basal ganglia, cerebellum, or pyramidal tracts, disrupts the normal communication between the brain and muscles. This disruption leads to altered reflex activity. For example, many children with CP exhibit **spasticity**, a condition characterized by increased muscle tone and exaggerated reflexes, especially the stretch reflex. This means that when a muscle is stretched, it contracts more strongly and more quickly than normal, which can cause stiffness and difficulty with movement[2][5].
One common reflex affected in CP is the **Babinski reflex**. Normally, this reflex disappears after infancy, but in children with CP, it may persist or reappear, indicating damage to the corticospinal tract, a key pathway for voluntary motor control[4]. The persistence of primitive reflexes like the Babinski reflex or the Moro reflex beyond infancy is a hallmark sign of neurological impairment in CP.
The **tonic stretch reflex threshold (TSRT)** is another important concept in understanding reflex abnormalities in CP. TSRT measures the point at which a muscle stretch triggers a reflex contraction. In CP, this threshold is often lowered, meaning muscles respond to smaller stretches with reflex contractions, contributing to spasticity and impaired voluntary movement[3].
Reflex abnormalities in CP are not uniform; they vary depending on the type and severity of CP. For instance:
– **Spastic CP**, the most common form, is marked by hyperactive reflexes and muscle stiffness.
– **Ataxic CP** affects balance and coordination, often with less pronounced reflex abnormalities but impaired fine motor control[2].
– **Dyskinetic CP** involves involuntary movements and fluctuating muscle tone, which can also alter reflex responses.
These abnormal reflexes interfere with normal motor development. Babies with CP often retain reflexes that typically disappear in early infancy, such as the **Moro reflex** or **tonic neck reflex**, which can hinder the development of voluntary motor skills like rolling, sitting, crawling, and walking[2][7]. The persistence of these reflexes can cause abnormal postures and movement patterns, making physical therapy and neurodevelopmental treatments essential for improving motor function[1][8].
Neurodevelopmental treatment (NDT) and other rehabilitation approaches aim to modulate these reflexes and improve motor control. Studies have shown that targeted physical therapy can reduce spasticity and improve gross motor functions by influencing reflex activity and muscle tone[1]. For example, NDT helps children with CP gain better control over their movements by promoting more normal reflex patterns and muscle activation.
In clinical practice, assessing reflexes is a key part of diagnosing and monitoring CP. Healthcare providers perform neurological exams that include testing reflexes to evaluate the extent of motor impairment and to guide treatment planning[2][6]. Reflex testing helps distinguish CP from other conditions and track progress over time.
In summary, cerebral palsy affects reflexes by causing abnormal, often exaggerated reflex responses due to brain damage affecting motor pathways. These altered reflexes contribute to muscle stiffness, impaired movement, and delayed motor milestones