Resveratrol, a natural compound found in foods like grapes, red wine, berries, and peanuts, has attracted significant attention for its potential to lower the risk of dementia, particularly Alzheimer’s disease. This interest stems from resveratrol’s ability to influence multiple biological pathways involved in brain aging and neurodegeneration, making it a promising candidate for protecting cognitive health.
At the core of dementia, especially Alzheimer’s disease, are complex processes such as the buildup of toxic proteins (amyloid-beta plaques and tau tangles), chronic inflammation in the brain, oxidative stress caused by harmful free radicals, and the gradual loss of neurons. Resveratrol appears to target many of these damaging mechanisms simultaneously, which is why it is considered a multi-faceted neuroprotective agent.
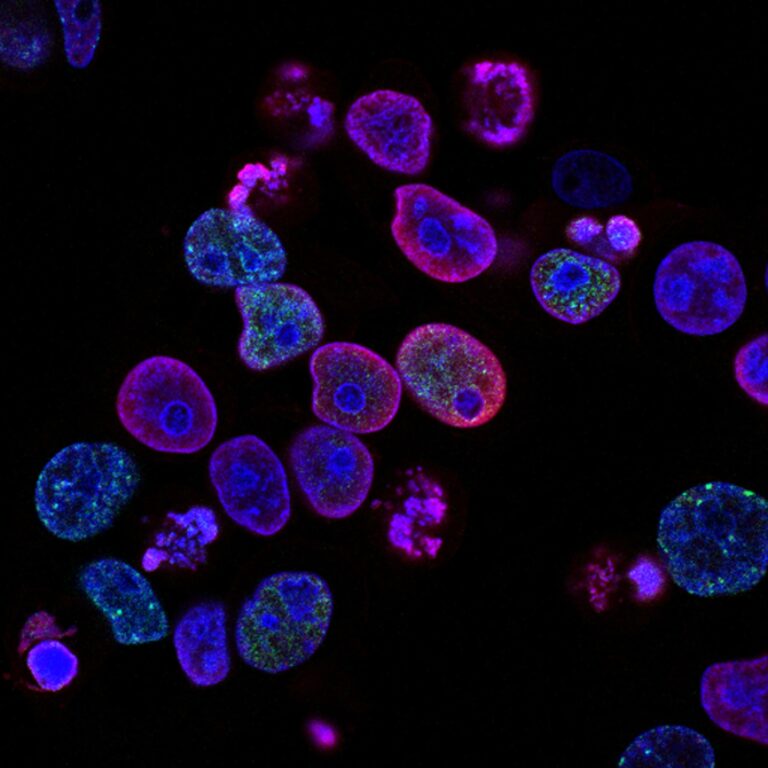
One of the key ways resveratrol may help is by activating a group of proteins called sirtuins, particularly SIRT1. These proteins are linked to longevity and cellular health. When activated, SIRT1 promotes the cleanup of damaged proteins and supports the survival of neurons, which can slow down or prevent the progression of dementia-related changes. This activation also helps reduce inflammation by suppressing the activity of microglia, the brain’s immune cells that, when overactive, contribute to neuroinflammation by releasing harmful molecules like IL-1β and TNF-α.
Resveratrol also acts as a powerful antioxidant. It helps neutralize free radicals—unstable molecules that damage cells and DNA—thereby reducing oxidative stress in the brain. This antioxidant effect is enhanced by resveratrol’s ability to boost the activity of the brain’s own defense enzymes, such as catalase, superoxide dismutase (SOD), and glutathione peroxidase. By strengthening these defenses, resveratrol protects neurons from oxidative damage, which is a major factor in cognitive decline.
Another important aspect of resveratrol’s action is its influence on the blood-brain barrier (BBB), a protective shield that controls what substances can enter the brain from the bloodstream. Resveratrol helps maintain the integrity of this barrier by protecting tight junction proteins and reducing the expression of molecules that promote inflammation and vascular damage. This preservation of the BBB is crucial because a compromised barrier allows harmful substances to enter the brain, exacerbating neurodegeneration.
Resveratrol also interferes with the formation and aggregation of amyloid-beta plaques, which are hallmark features of Alzheimer’s disease. By reducing the amount of amyloid-beta available to form toxic clumps, resveratrol may slow the progression of plaque buildup. Additionally, it inhibits the activation of inflammasomes—protein complexes that trigger inflammatory responses—thereby further reducing neuroinflammation.
Beyond these molecular effects, resveratrol influences signaling pathways such as the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway, which regulates inflammation and immune responses in the brain. By modulating this pathway, resveratrol helps keep inflammation in check, protecting neurons from damage.
Despite these promising mechanisms, there are challenges in translating resveratrol’s benefits into effective dementia prevention or treatment. One major hurdle is its poor bioavailability—meaning that when consumed, only a small fraction of resveratrol actually reaches the brain in an active form. The blood-brain barrier, while protective, also limits the amount of resveratrol that can enter brain tissue. Researchers are exploring ways to improve delivery, such as developing resveratrol derivatives or using specialized carriers to enhance brain uptake.
In animal and preclinical studies, resveratrol has consistently shown protective effects against cognitive decline, improving memory and reducing markers of brain inflammation and oxidative stress. Human clinical trials, however, have produced mixed results so far. Some studies report improvements in cognitive function or biomarkers related to brain health, while others find minimal or no significant effects. These discrepancies ma