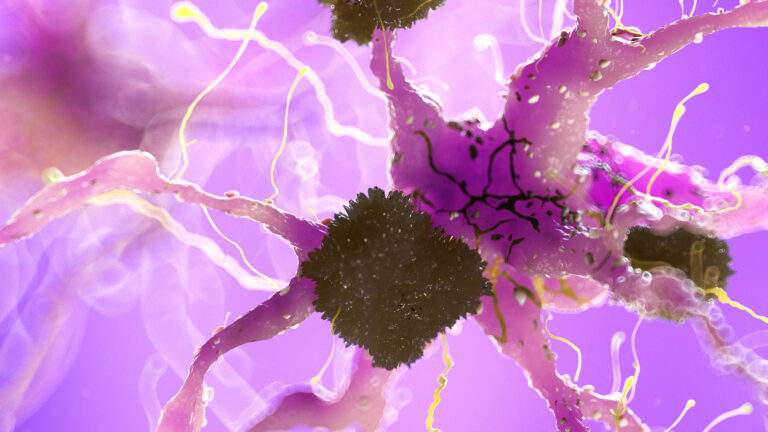
Magnetic Resonance Imaging (MRI) scans can indeed show brain changes in Huntington’s disease, particularly structural alterations that occur as the disease progresses. Huntington’s disease is a genetic neurodegenerative disorder characterized by the gradual breakdown of neurons in specific brain regions, especially the basal ganglia, which includes the caudate nucleus and putamen. These areas are crucial for controlling movement, cognition, and emotion, and their degeneration leads to the hallmark symptoms of Huntington’s disease such as involuntary movements, cognitive decline, and psychiatric disturbances.
MRI is a powerful imaging tool that provides detailed pictures of brain anatomy without using radiation. In Huntington’s disease, MRI scans typically reveal **atrophy**, or shrinkage, of the caudate nucleus and putamen. This atrophy reflects the loss of neurons and the resulting reduction in brain tissue volume in these regions. The degree of atrophy often correlates with disease severity and progression. Early in the disease, MRI may show subtle changes, but as the disease advances, the atrophy becomes more pronounced and easier to detect.
Beyond visible atrophy, MRI can also be used to assess other brain changes indirectly related to Huntington’s disease. For example, advanced MRI techniques such as diffusion tensor imaging (DTI) can detect microstructural changes in white matter tracts, which are the brain’s communication pathways. These changes may occur before significant atrophy is visible and can provide insights into how the disease disrupts brain connectivity.
Functional imaging techniques related to MRI, like functional MRI (fMRI) and magnetic resonance spectroscopy (MRS), can also reveal changes in brain activity and metabolism in Huntington’s disease. Although these are not standard clinical tools for diagnosis, they are valuable in research settings to understand the disease’s impact on brain function. For instance, MRS can detect alterations in brain metabolites that reflect neuronal loss or dysfunction.
In addition to MRI, other imaging modalities such as positron emission tomography (PET) scans have shown reduced glucose metabolism in the basal ganglia of Huntington’s patients, indicating impaired brain energy use. However, MRI remains the primary imaging method for visualizing structural brain changes.
It is important to note that while MRI can show characteristic brain changes in Huntington’s disease, it cannot diagnose the disease on its own. Diagnosis relies on a combination of clinical evaluation, family history, genetic testing for the huntingtin gene mutation, and imaging findings. MRI is most useful for supporting the diagnosis, monitoring disease progression, and ruling out other conditions that might mimic Huntington’s symptoms.
In summary, MRI scans can clearly demonstrate brain changes in Huntington’s disease, especially the atrophy of the caudate nucleus and putamen. These changes reflect the underlying neuronal loss and are key markers of disease progression. Advanced MRI techniques further enhance the ability to detect subtle brain alterations, making MRI an essential tool in the study and clinical management of Huntington’s disease.