MRI scans can indeed misinterpret pacemaker artifacts, and understanding why this happens requires a look into both the nature of MRI technology and the characteristics of pacemakers.
Magnetic Resonance Imaging (MRI) is a powerful diagnostic tool that uses strong magnetic fields and radio waves to create detailed images of the inside of the body. It excels at showing soft tissues, organs, and blood vessels with high clarity. However, MRI machines are highly sensitive to metal objects and electronic devices inside the body, such as pacemakers. Pacemakers are small electronic devices implanted in patients to regulate heart rhythms, and they contain metal components and electronic circuits that can interact with the MRI’s magnetic field.
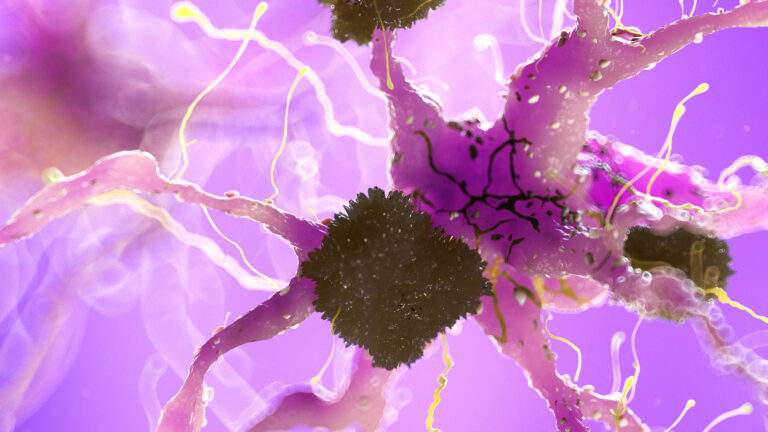
When a patient with a pacemaker undergoes an MRI scan, the metal parts of the pacemaker can cause distortions in the magnetic field. These distortions appear as artifacts on the MRI images. Artifacts are essentially errors or anomalies in the image that do not represent actual anatomical structures but are caused by interference. In the case of pacemakers, these artifacts can look like bright or dark spots, streaks, or distortions that obscure the surrounding tissues.
The misinterpretation happens because these artifacts can mimic or hide real anatomical or pathological features. For example, an artifact might be mistaken for a lesion, a blood clot, or other abnormalities, leading to incorrect diagnoses. Conversely, important clinical details might be obscured by the artifact, causing a missed diagnosis. This is particularly critical in cardiac imaging, where precise visualization of heart structures is essential.
Several factors influence the extent and nature of pacemaker artifacts in MRI scans:
– **Type of pacemaker:** Older pacemakers tend to cause more significant artifacts because they were not designed with MRI compatibility in mind. Modern MRI-conditional pacemakers are engineered to minimize interference, but artifacts can still occur.
– **Location of the pacemaker:** The closer the pacemaker is to the area being imaged, the more likely it is to cause artifacts that affect image quality.
– **MRI scanning parameters:** The strength of the magnetic field (measured in Tesla), the imaging sequences used, and the orientation of the scan can all affect the visibility and severity of artifacts.
– **Patient anatomy and positioning:** Individual differences in body composition and how the patient is positioned during the scan can influence artifact appearance.
To reduce the risk of misinterpretation, radiologists and technicians use several strategies:
– **Specialized MRI protocols:** Adjusting scanning parameters to reduce artifact size and intensity, such as using sequences less sensitive to metal interference.
– **Artifact reduction techniques:** Advanced software algorithms can sometimes correct or minimize artifacts during image reconstruction.
– **Alternative imaging methods:** When MRI artifacts are too severe, other imaging modalities like CT scans or ultrasound may be used to complement or replace MRI.
– **Careful clinical correlation:** Radiologists interpret MRI findings in the context of the patient’s history, symptoms, and other test results to avoid mistaking artifacts for pathology.
Despite these measures, the presence of pacemaker artifacts remains a significant challenge in MRI imaging. It requires expertise and caution to distinguish true anatomical features from artifact-induced distortions. As MRI technology and pacemaker design continue to evolve, the goal is to further reduce these artifacts and improve diagnostic accuracy for patients with implanted devices.