Magnetic Resonance Imaging (MRI) scans have become a crucial tool in understanding brain structure and function, especially in complex conditions like dementia and depression. When it comes to detecting depression in dementia patients, MRI offers valuable insights but also faces significant challenges.
Dementia is a broad term describing a decline in cognitive function severe enough to interfere with daily life, often caused by neurodegenerative diseases such as Alzheimer’s. Depression frequently co-occurs with dementia, complicating diagnosis and treatment. Differentiating depressive symptoms from dementia-related cognitive decline is difficult because both conditions can affect memory, attention, and executive function. This overlap makes clinical diagnosis challenging, and objective tools like MRI are being explored to improve accuracy.
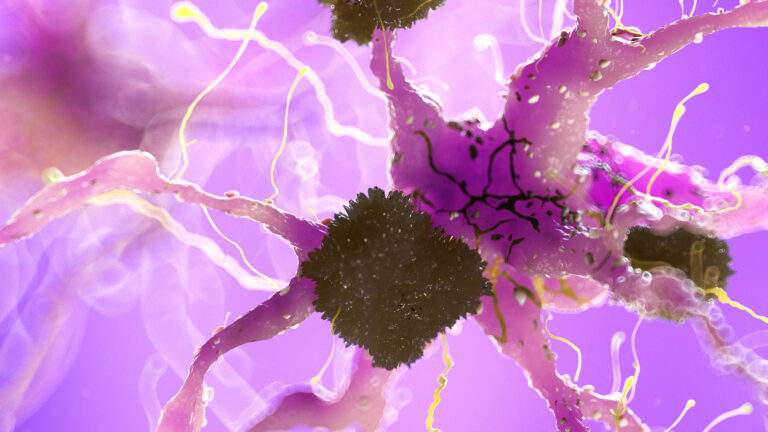
MRI scans provide detailed images of brain anatomy and can also be used to assess brain activity and connectivity through advanced techniques. In dementia patients, MRI can reveal patterns of brain atrophy (shrinkage), changes in white matter, and other structural abnormalities. These changes often correlate with the severity and type of dementia. For depression, MRI studies have identified alterations in brain regions involved in mood regulation, such as the prefrontal cortex, hippocampus, insula, and temporal lobes.
One of the key ways MRI can contribute to detecting depression in dementia is by identifying specific brain changes associated with depressive symptoms. For example, research has shown that patients with major depressive disorder exhibit altered connectivity and entropy (a measure of complexity) in regions like the insula and superior temporal cortex. These changes relate to subjective cognitive complaints and impaired executive function, which are also common in dementia. Such findings suggest that MRI could help distinguish depressive cognitive impairment from dementia-related decline by highlighting unique patterns of brain activity and connectivity.
Moreover, advanced MRI techniques like quantitative susceptibility mapping (QSM) can measure brain iron levels, which have been linked to neurodegeneration and cognitive impairment. Elevated iron in certain brain areas may exacerbate both dementia and depression symptoms by promoting oxidative stress and neuronal damage. Detecting these changes noninvasively could provide early warning signs of cognitive decline and mood disorders in at-risk individuals.
However, despite these promising developments, MRI alone cannot definitively diagnose depression in dementia patients. The brain changes seen in depression and dementia often overlap, and factors like medication, disease stage, and individual variability affect MRI findings. Additionally, depression in dementia may present differently than in the general population, with symptoms sometimes masked by cognitive deficits.
To improve diagnostic accuracy, MRI findings are increasingly combined with clinical assessments, neuropsychological testing, and other biomarkers such as cerebrospinal fluid analysis or PET scans. This multimodal approach helps clinicians better understand the complex interplay between depression and dementia.
In clinical practice, MRI can support the detection of depression in dementia by:
– Revealing brain atrophy patterns that correlate with depressive symptoms.
– Identifying altered functional connectivity in mood-related brain regions.
– Measuring brain iron accumulation linked to neurodegenerative and mood disorders.
– Providing objective data to complement subjective cognitive complaints and clinical evaluations.
Nevertheless, the interpretation of MRI results requires expertise and should be integrated with comprehensive patient assessments. Ongoing research aims to refine MRI techniques and develop reliable biomarkers to distinguish depression from dementia-related cognitive impairment more clearly.
In summary, MRI scans offer valuable but not definitive insights into depression in dementia patients. They help identify brain changes associated with mood and cognitive symptoms, contributing to a more nuanced understanding of these overlapping conditions. Continued advances in imaging technology and combined diagnostic approaches hold promise for earlier and more accurate detection, ultimately improving patient care.