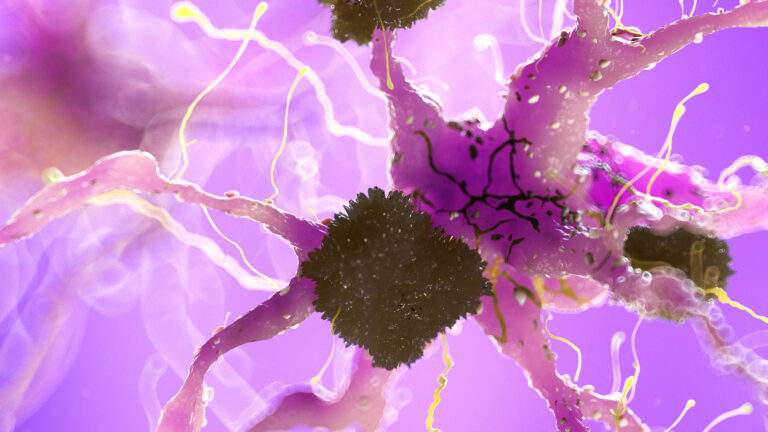
Magnetic Resonance Imaging (MRI) scans are a crucial tool in diagnosing and monitoring brain conditions, including dementia. However, performing MRI scans on patients with dementia who exhibit restlessness or agitation presents significant challenges. Adapting MRI procedures for restless dementia patients is both necessary and complex, involving modifications in technology, patient management strategies, and clinical protocols to ensure accurate imaging while minimizing distress.
Dementia often leads to cognitive decline accompanied by behavioral symptoms such as agitation, confusion, and restlessness. These symptoms can make it difficult for patients to remain still during an MRI scan—a requirement because movement can blur images and reduce diagnostic quality. Since MRI machines use strong magnetic fields and require the patient to lie still inside a confined space for extended periods (often 20-60 minutes), restless behavior complicates the process.
To adapt MRI scans for restless dementia patients, several approaches have been developed or proposed:
1. **Shortened Scan Times**
Advances in MRI technology allow faster image acquisition through techniques like parallel imaging or compressed sensing. Shorter scan times reduce the duration a patient must remain still, decreasing discomfort and likelihood of movement artifacts.
2. **Motion Correction Technologies**
New software algorithms can detect motion during scanning and correct images accordingly. Real-time motion tracking systems using cameras or sensors help adjust data collection dynamically to compensate for small movements.
3. **Patient Preparation & Comfort Measures**
Preparing patients before scanning includes explaining the procedure simply if possible; however, many with advanced dementia may not comprehend fully. Using calming environments—soft lighting, noise reduction headphones playing soothing sounds—and positioning aids like cushions help minimize anxiety-induced movements.
4. **Sedation or Anesthesia**
In some cases where agitation is severe enough that cooperation cannot be achieved otherwise, mild sedation may be administered under medical supervision to keep the patient calm during scanning without compromising safety significantly.
5. **Specialized Protocols & Staff Training**
Radiology teams trained specifically in handling cognitively impaired individuals use gentle communication techniques tailored to each patient’s needs while ensuring safety protocols are strictly followed throughout imaging sessions.
6. **Alternative Imaging Modalities When Necessary**
If an adequate MRI cannot be obtained due to excessive movement despite adaptations, other neuroimaging methods such as CT scans might be used as alternatives though they provide less detailed soft tissue contrast compared with MRIs.
7. **Use of Functional Imaging Techniques Adapted for Dementia Research**
Functional MRIs (fMRI) that assess brain activity patterns have been adapted with resting-state protocols requiring minimal active participation from subjects; these may offer insights into neural connectivity changes even when full cooperation isn’t feasible.
8. **Integration of Multimodal Approaches**
Combining structural MRIs with PET scans or cerebrospinal fluid analysis provides complementary information about brain pathology without relying solely on perfect structural images from restless patients alone.
The goal behind these adaptations is twofold: first—to obtain high-quality diagnostic images critical for assessing disease progression or response to treatment; second—to ensure that the experience does not exacerbate distressing symptoms common among dementia sufferers such as fear or confusion caused by unfamiliar environments like an MRI suite.
In practical terms:
– Clinics increasingly invest in faster scanners capable of whole-brain imaging within minutes.
– Motion correction software continues evolving rapidly alongside hardware improvements.
– Sedation policies balance risks versus benefits carefully since elderly dementia patients often have comorbidities increasing anesthesia risks.
– Caregivers’ presence during scanning sometimes helps soothe anxious individuals but requires strict safety measures due to magnetic field hazards.
– Research into non-invasive biomarkers detectable via modified imaging sequences aims at reducing dependence on prolonged static positioning altogether over time.
Ultimately adapting MRIs for restless dementia patients involves a multidisciplinary effort combining technological innovation with compassionate clinical care tailored specifically toward this vulnerable population’s unique needs—allowing clinicians better tools while respecting patient dignity amid challenging circumstances inherent in neurodegenerative diseases marked by behavioral disturbance