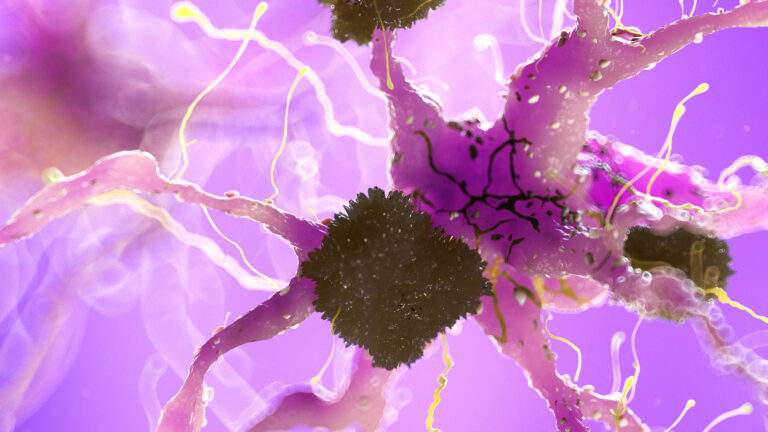
Functional MRI (fMRI) can detect early changes in brain activity associated with Alzheimer’s disease, making it a promising tool for identifying the disease before significant symptoms appear. Unlike traditional MRI, which shows structural brain changes, fMRI measures brain activity by detecting changes in blood flow, reflecting neural function. This allows researchers and clinicians to observe how different brain regions communicate and function during rest or cognitive tasks, which can reveal subtle disruptions caused by early Alzheimer’s pathology.
In the earliest stages of Alzheimer’s, before noticeable memory loss or cognitive decline, the brain undergoes functional changes that fMRI can capture. These include altered connectivity within and between key brain networks involved in memory, attention, and sensory processing. For example, fMRI studies have shown that individuals with subjective cognitive decline—a state where people feel their memory is worsening but perform normally on tests—exhibit increased functional connectivity in certain brain regions. This may represent a compensatory mechanism where the brain tries to maintain function despite early damage. As the disease progresses to mild cognitive impairment (MCI), these connectivity patterns often decrease, correlating with worsening cognitive performance.
One important network often studied with fMRI in Alzheimer’s is the default mode network (DMN), which is active during rest and involved in self-referential thinking and memory. Early Alzheimer’s is associated with disrupted connectivity in the DMN and its interaction with other networks like the dorsal attention network. These disruptions can serve as biomarkers indicating the presence of Alzheimer’s pathology even before clinical symptoms are evident.
Advanced computational models combining fMRI data with machine learning techniques have improved the ability to classify and stage Alzheimer’s disease. For instance, integrating convolutional neural networks (CNNs) and long short-term memory (LSTM) networks allows for capturing both spatial and temporal features of brain activity, enhancing early detection accuracy. These models can differentiate between normal aging, early mild cognitive impairment, and Alzheimer’s disease, potentially enabling earlier intervention.
Beyond functional connectivity, specialized MRI techniques related to fMRI, such as quantitative susceptibility mapping (QSM), can detect abnormal iron accumulation in the brain, which is linked to Alzheimer’s progression. Iron overload contributes to oxidative stress and neuronal damage, and its measurement complements fMRI findings by providing additional insight into disease mechanisms.
fMRI also helps explore sensory-related changes in Alzheimer’s, such as olfactory dysfunction. Altered functional connectivity in olfactory networks has been observed in individuals at risk for Alzheimer’s, correlating with both smell deficits and cognitive decline. This suggests that fMRI can detect early neural changes related to sensory processing that precede or accompany cognitive symptoms.
Overall, fMRI provides a window into the dynamic brain changes occurring in the earliest phases of Alzheimer’s disease. By revealing altered brain activity and connectivity patterns before significant structural damage or clinical symptoms arise, fMRI holds great potential for early diagnosis. Early detection is crucial because it opens the door to timely therapeutic interventions that may slow disease progression and improve quality of life. As research advances, combining fMRI with other imaging modalities and computational approaches will likely enhance its role as a sensitive and non-invasive biomarker for Alzheimer’s disease activity changes at the earliest stages.