Iodine deficiency during pregnancy can increase the risk of neurodevelopmental disorders in children, including autism spectrum disorder (ASD), though the relationship is complex and not fully established. Iodine is a critical mineral necessary for the production of thyroid hormones, which are essential for normal fetal brain development. When a pregnant woman has insufficient iodine intake, it can lead to maternal hypothyroxinemia (low thyroid hormone levels), which has been linked to impaired fetal brain development and increased risk of cognitive deficits and neurodevelopmental disorders such as autism[1][2].
**Role of Iodine in Pregnancy and Brain Development**
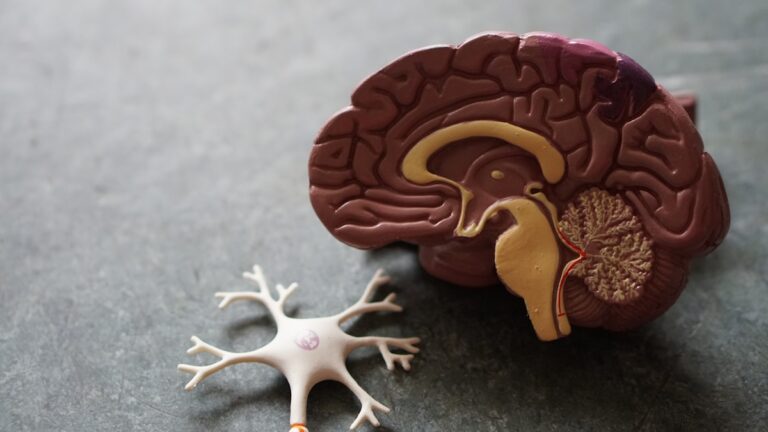
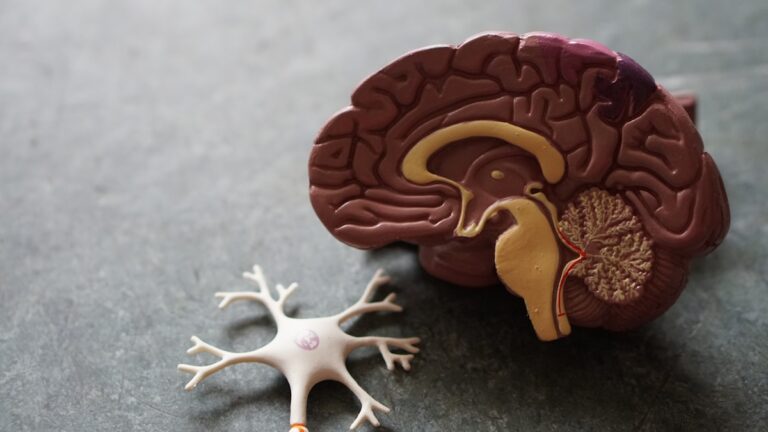
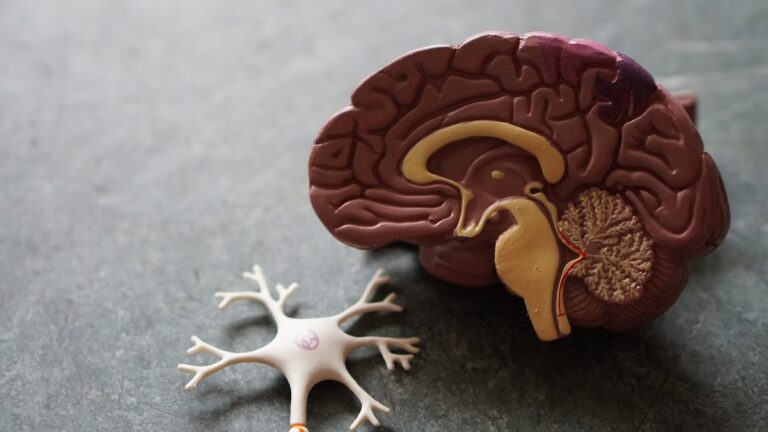
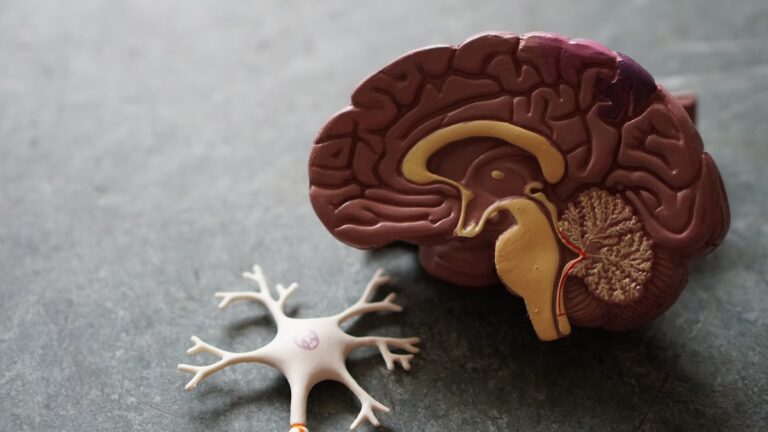
Iodine is vital for synthesizing thyroid hormones—thyroxine (T4) and triiodothyronine (T3)—which regulate many aspects of fetal growth and brain maturation. During early pregnancy, the fetus depends entirely on maternal thyroid hormones, as its own thyroid gland is not fully functional until mid-gestation. If the mother’s iodine intake is inadequate, thyroid hormone production decreases, potentially disrupting critical neurodevelopmental processes such as neuronal migration, myelination, and synaptogenesis[1][2].
Severe iodine deficiency during pregnancy is well-known to cause cretinism, a condition characterized by profound intellectual disability and physical abnormalities. Even mild to moderate iodine deficiency has been associated with lower IQ scores and developmental delays in children. One study cited a 15-point IQ reduction in children born to iodine-deficient mothers[1].
**Evidence Linking Iodine Deficiency to Autism Risk**
Autism spectrum disorder is a complex neurodevelopmental condition with multifactorial causes, including genetic and environmental factors. Among prenatal environmental risks, maternal thyroid hormone deficiency due to iodine deficiency is hypothesized to contribute to autism risk. Thyroid hormone insufficiency during the first trimester (weeks 8–12) is particularly critical because this period involves early brain patterning and neuronal differentiation[2].
A 2021 meta-analysis highlighted various prenatal risk factors for autism, including maternal thyroid problems leading to thyroxine deficiency. Since iodine deficiency is a leading cause of hypothyroxinemia, it is implicated as a potential contributor to autism development. However, this hypothesis remains under investigation and has not been conclusively proven[2].
Additional indirect evidence comes from clinical observations of children with autism who have restricted diets lacking iodine-rich foods (such as seafood, dairy, and eggs), leading to iodine deficiency and thyroid dysfunction. For example, a pediatric endocrinologist reported cases of children with autism and goiter due to iodine deficiency, which improved with iodine supplementation[4].
**Broader Context of Maternal Nutrition and Neurodevelopment**
Iodine deficiency is one of several nutritional factors influencing fetal brain development. Deficiencies in other micronutrients, such as folic acid, have also been linked to increased risks of neurodevelopmental disorders including autism and ADHD. Folic acid deficiency can alter DNA methylation patterns, affecting gene expression critical for brain development[3].
Maternal malnutrition, obesity, diabetes, autoimmune diseases, and infections during pregnancy are additional prenatal factors associated with increased autism risk. These conditions can cause inflammation or disrupt immune signaling, further complicating fetal neurodevelopment[2].
**Prevalence and Public Health Implications**
Despite global efforts to reduce iodine deficiency through iodized salt programs, iodine deficiency remains a public health concern, especially in low- and middle-income countries an