The question of whether **prenatal stress hormones trigger Asperger’s syndrome** touches on a complex interplay between prenatal environmental factors and neurodevelopmental outcomes. Asperger’s syndrome, now classified under Autism Spectrum Disorder (ASD) in the DSM-5, is characterized by difficulties in social interaction and restricted, repetitive behaviors, but without significant delays in language or cognitive development.
**Prenatal stress hormones, particularly cortisol, have been studied extensively for their potential impact on fetal brain development and subsequent risk of ASD, including Asperger’s.** Cortisol is a glucocorticoid hormone released by the adrenal glands in response to stress, and during pregnancy, maternal cortisol levels naturally increase to support fetal development. However, excessive or prolonged elevations in maternal cortisol—often a marker of prenatal stress—may influence the developing brain in ways that increase the risk of neurodevelopmental disorders.
### How Prenatal Stress Hormones Might Influence ASD Risk
1. **Maternal Cortisol and Fetal Brain Development**
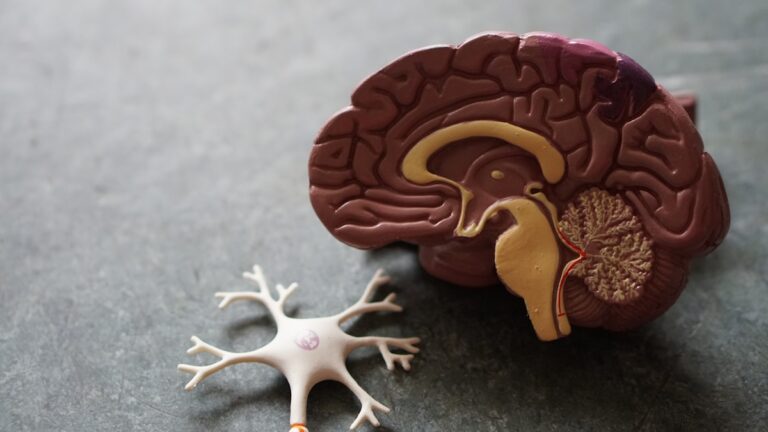
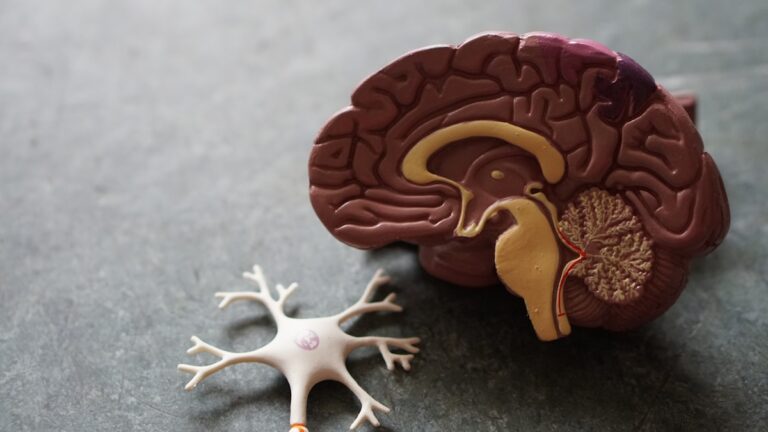
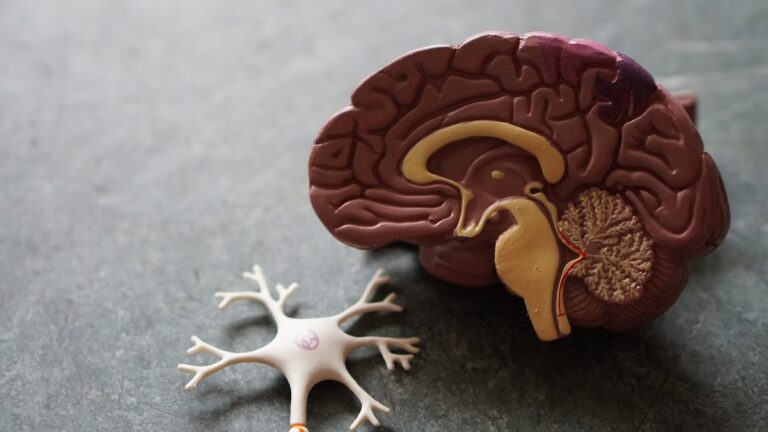
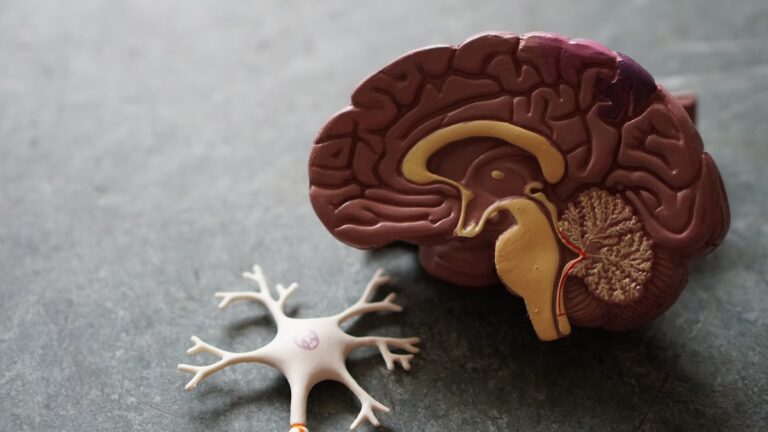
During pregnancy, maternal cortisol crosses the placenta and can affect the fetal hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress responses. Elevated prenatal cortisol exposure has been linked to alterations in brain regions critical for social behavior and cognition, such as the amygdala and prefrontal cortex. These brain changes may underlie some ASD traits, including those seen in Asperger’s syndrome [1].
2. **Evidence Linking Maternal Stress and ASD**
Several studies have found associations between high maternal cortisol levels during pregnancy and increased risk of ASD in offspring, particularly in males. For example, research indicates that variations in maternal cortisol correlate with ASD risk, suggesting that prenatal stress hormones may contribute to atypical neurodevelopment [1][3]. However, these findings are correlational and do not establish direct causation.
3. **Mechanisms: Immune Activation and Inflammation**
Prenatal stress can also trigger maternal immune activation, leading to elevated pro-inflammatory cytokines that cross the placenta and disrupt fetal brain development. This immune response may interact with cortisol effects, compounding the risk of ASD [1]. The timing of stress exposure during pregnancy is critical; early gestational stress may affect neural tube formation, while later stress may impact synapse formation and cortical organization.
4. **Genetic and Environmental Interactions**
ASD, including Asperger’s, is widely recognized as a multifactorial condition involving both genetic predispositions and environmental influences. Prenatal stress hormones may act as environmental triggers that interact with genetic vulnerabilities to increase ASD risk. This gene-environment interplay complicates the picture and means that prenatal cortisol alone is unlikely to be the sole cause [1].
### What Does This Mean for Asperger’s Specifically?
Asperger’s syndrome shares core features with other forms of ASD but is distinguished by the absence of language delay and intellectual disability. The research on prenatal stress hormones often addresses ASD broadly rather than Asperger’s specifically. However, since Asperger’s is part of the autism spectrum, it is reasonable to infer that prenatal cortisol and stress-related mechanisms could similarly influence its development.
### Additional Factors Influencing Prenatal Stress and ASD Risk
– **Maternal Anxiety and Hormonal Changes**
Pregnancy itself causes hormonal fluctuations, including increased cortisol production (two to four times higher than normal), which can heighten maternal anxiety an