Multiple sclerosis (MS) is a chronic autoimmune disease where the immune system mistakenly attacks the protective covering of nerve fibers in the central nervous system, leading to inflammation, damage, and neurological disability. Traditional MS drugs primarily focus on modulating or suppressing the immune response to reduce relapses and slow progression. However, stem cell treatments have emerged as a promising alternative or complementary approach that may offer different benefits and risks compared to conventional medications.
Stem cell therapies for MS generally involve using cells that can modulate the immune system and potentially repair damaged nervous tissue. Two main types of stem cell approaches are being explored: hematopoietic stem cell transplantation (HSCT) and mesenchymal stem cell (MSC) therapy.
Hematopoietic stem cell transplantation involves wiping out a patient’s existing immune system with high-dose chemotherapy or immunosuppressive agents, then reintroducing their own previously collected blood-forming stem cells to rebuild a new immune system. The idea is that this “resets” the immune response so it no longer attacks myelin or nerve tissue. Clinical trials have shown encouraging results with HSCT in patients with aggressive relapsing forms of MS who do not respond well to standard drugs. Many patients experience prolonged periods without disease progression or relapses after HSCT, sometimes lasting several years. However, this procedure carries significant risks due to intense immunosuppression—such as infections, organ toxicity, and treatment-related mortality—which limits its use mainly to severe cases under specialized care.
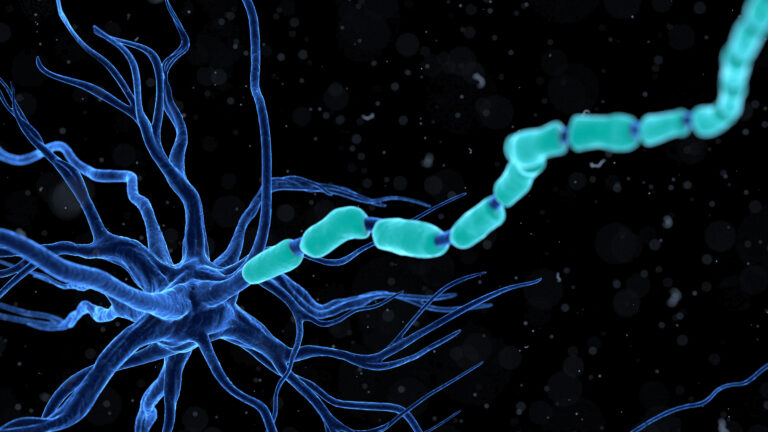
Mesenchymal stem cells are another type being studied for MS treatment because they possess immunomodulatory properties—they can calm down harmful inflammation—and neuroprotective effects—they may help protect neurons from further damage and support repair processes like remyelination (restoring myelin). MSCs can be derived from various tissues such as bone marrow or adipose tissue and administered intravenously or directly into cerebrospinal fluid in clinical trials. Early-phase studies suggest MSC therapy is generally safe with fewer serious side effects than HSCT; some patients show improvements in neurological function scores and reduced lesion activity on MRI scans after treatment. Still, long-term efficacy data are limited; researchers continue working on optimizing dosing protocols and understanding which patients benefit most.
In contrast, traditional MS drugs include disease-modifying therapies (DMTs) such as interferons, monoclonal antibodies targeting specific immune cells like B-cells (e.g., ocrelizumab), oral agents affecting lymphocyte trafficking (e.g., fingolimod), among others. These medications aim primarily at reducing relapse frequency by suppressing parts of the immune response but do not repair existing nerve damage directly nor fully halt progression in all cases.
When comparing safety profiles:
– **MS Drugs**: Generally well-studied over decades with known side effect profiles ranging from mild flu-like symptoms to increased infection risk depending on drug potency; ongoing monitoring required but usually manageable outpatient treatments.
– **HSCT**: Higher upfront risk due to intensive chemotherapy causing potential life-threatening complications; requires hospitalization under expert centers; however offers possibility of durable remission especially for refractory cases.
– **MSC Therapy**: Appears safer than HSCT based on current evidence since it does not require full ablation of immunity; adverse events mostly mild infusion reactions reported so far though long-term safety still under evaluation.
Effectiveness-wise:
– Conventional DMTs reduce relapse rates significantly but often only partially slow disability accumulation.
– HSCT shows promise for more profound resetting of disease course but reserved for aggressive forms due to risks.
– MSC treatments hold potential both for modulating immunity *and* promoting neural repair mechanisms—a dual action lacking in most current drugs—but remain experimental pending larger confirmatory trials.
In summary terms without oversimplifying:
Stem cell treatments represent an exciting frontier offering potentially greater benefits by addressing both inflammatory activity *and* neurodegeneration inherent in MS pathology—something traditional drugs cannot fully achieve alone yet come with varying degrees of ris