Menopause symptoms improve with exercise for some women but not others due to a complex interplay of biological, psychological, and lifestyle factors that influence how each individual’s body responds to physical activity during this hormonal transition.
Menopause is marked by a significant decline in estrogen and progesterone, hormones that regulate many bodily functions. This hormonal shift causes symptoms such as hot flashes, night sweats, mood swings, sleep disturbances, weight gain, and muscle loss. Exercise can help alleviate many of these symptoms by triggering beneficial physiological changes, but the degree of improvement varies widely among women.
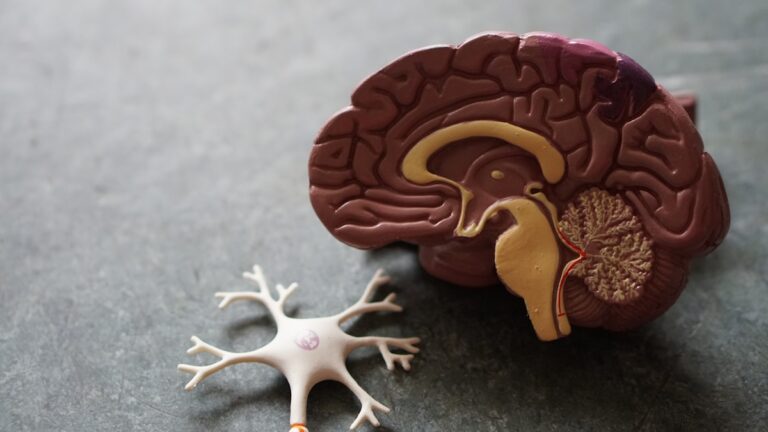
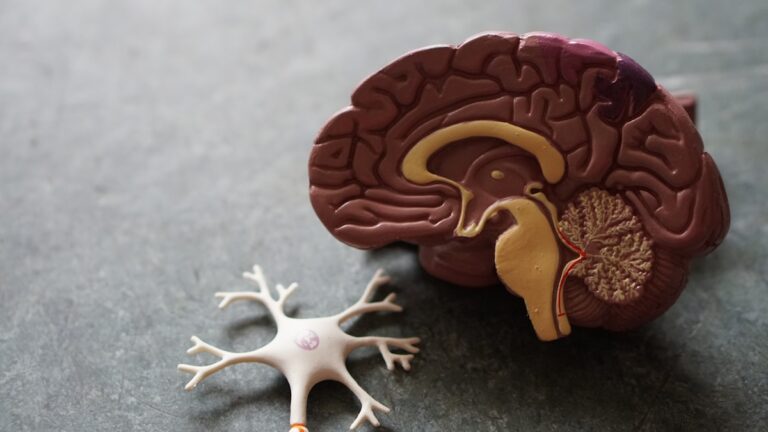
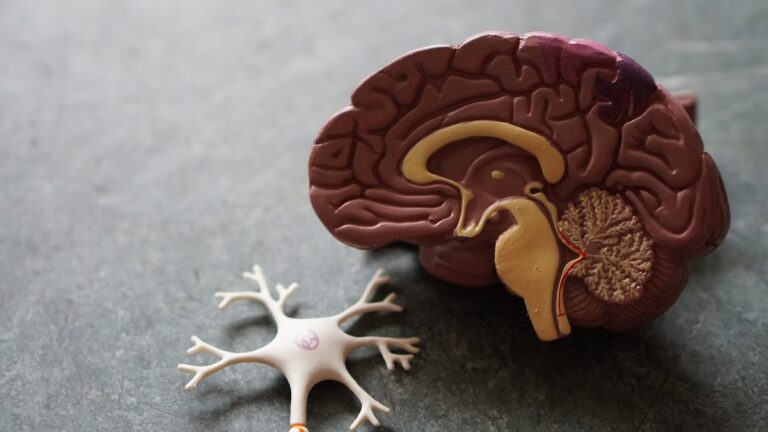
One key reason exercise helps is the release of endorphins, natural chemicals in the brain that improve mood and reduce pain perception. These “feel-good hormones” can ease mood swings, anxiety, and depression commonly experienced during menopause. Exercise also improves sleep quality by regulating circadian rhythms and reducing insomnia, which is often worsened by menopausal changes. Cardiovascular workouts enhance heart health and metabolism, counteracting the tendency for weight gain and fat accumulation around the abdomen that menopause promotes. Resistance training helps preserve muscle mass and bone density, which decline due to lower estrogen levels, reducing risks of osteoporosis and frailty.
However, not all women experience these benefits equally. Differences in genetics, baseline fitness levels, and hormone receptor sensitivity can influence how the body reacts to exercise. For example, some women may have a more robust endorphin response, leading to greater mood improvements, while others may have less sensitivity to these effects. The type, intensity, and frequency of exercise also matter. High-intensity workouts might trigger hot flashes or fatigue in some women, whereas moderate, consistent exercise tends to be more beneficial. Women who focus on strength training often report better energy and reduced anxiety compared to those who do mostly high-intensity interval training or excessive cardio.
Lifestyle factors such as diet, stress levels, sleep quality, and body composition also play a role. Women with higher body fat percentages may experience more severe symptoms, and while exercise can help reduce fat, it may take longer or require dietary changes to see symptom relief. Stress can exacerbate symptoms like hot flashes, and since exercise is a stress-reliever, those who manage stress well may notice more symptom improvement. Conversely, women under chronic stress or with poor sleep may find exercise less effective or even triggering for some symptoms.
Psychological factors and personal attitudes toward exercise influence outcomes too. Women who enjoy their workouts and feel motivated are more likely to maintain a consistent routine, which is crucial for symptom management. Those who find exercise stressful or uncomfortable may not gain the same benefits. Additionally, menopausal symptoms themselves can limit exercise ability—joint pain, fatigue, or mood disturbances may reduce motivation or capacity to engage in physical activity, creating a cycle where symptoms persist or worsen.
The type of exercise also matters. Weight-bearing and resistance exercises are particularly effective for bone and muscle health, while mind-body practices like yoga and tai chi can reduce stress and improve sleep. Stretching and mobility work help with stiffness and joint pain, common complaints during menopause. Women who incorporate a variety of exercise types tailored to their needs often see better overall symptom relief.
In some cases, exercise might not improve symptoms because the underlying hormonal imbalance is too severe or because other health conditions interfere. For example, women with thyroid disorders, chronic fatigue syndrome, or depression may not respond to exercise in the same way. Hormone replacement therapy or other medical treatments might be necessary to complement lifestyle changes.
Ultimately, the variability in menopause symptom improvement with exercise comes down to individual differences in biology, lifestyle, and the nature of the exercise itself. Finding the right balance of activity that fits one’s body, preferences, and symptom profile is essential. This often requires experimentation, professional guidance, and a holistic approach that includes stress management, nutrition, and adequate rest alongside physical activity.