Menopause symptoms often feel worse in winter because the cold weather, shorter daylight hours, and environmental changes interact with the hormonal shifts women experience during this time, amplifying discomfort and symptom severity. The drop in estrogen during menopause affects many body systems, and winter conditions tend to exacerbate these effects in several ways.
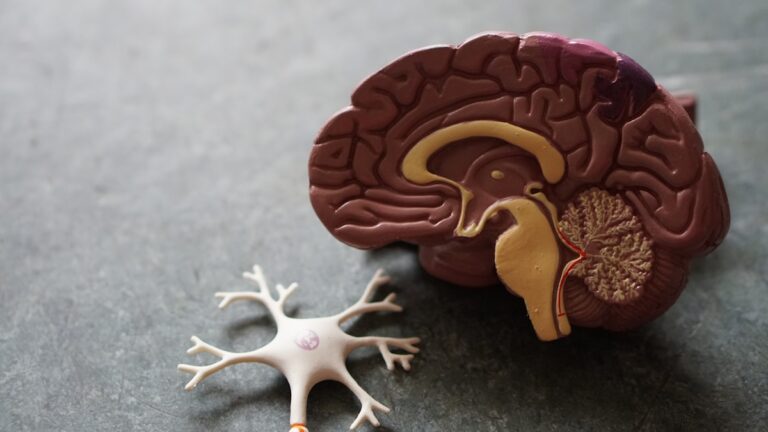
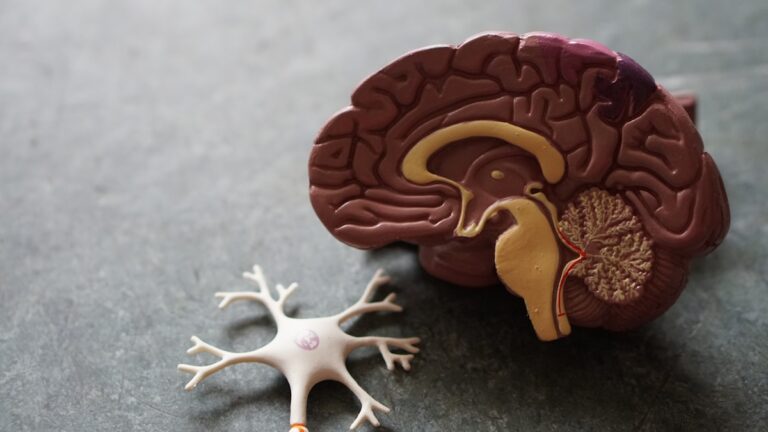
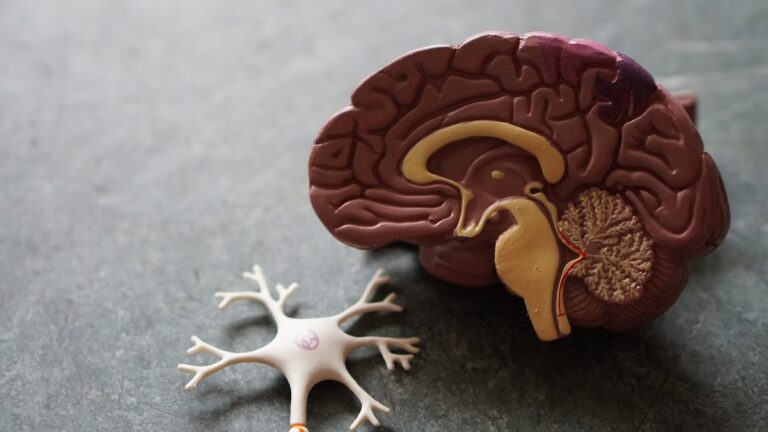
One major factor is the body’s impaired ability to regulate temperature during menopause. Estrogen decline disrupts the hypothalamus, the brain region that controls body temperature, causing hot flashes and night sweats. In winter, the frequent moving between cold outdoor air and warm indoor heating causes rapid temperature changes that can trigger or worsen hot flashes. This makes managing these sudden heat surges more difficult than in milder seasons.
Cold weather also worsens joint pain and stiffness, which are common menopause complaints. Estrogen helps maintain joint lubrication and bone density, so its decline leads to increased joint discomfort. The cold, damp air of winter tightens muscles and stiffens joints, intensifying aches and pains that might be mild or manageable during warmer months.
Skin dryness is another symptom aggravated by winter. Menopause reduces skin moisture and elasticity, and the dry indoor heating combined with cold outdoor air strips the skin of natural oils, leading to itchiness, flaking, and irritation. This dryness can also make the skin more sensitive and prone to cracking.
Sleep disturbances, already common in menopause due to night sweats and hormonal fluctuations, become more pronounced in winter. The combination of warm bedding, night sweats, and dry air creates an uncomfortable environment that disrupts restful sleep. Additionally, shorter daylight hours reduce exposure to natural light, which can interfere with circadian rhythms and melatonin production, further disturbing sleep patterns.
Mood changes and energy dips are often worse in winter due to the combined effects of hormonal shifts and seasonal factors. Reduced sunlight can lead to lower vitamin D levels and contribute to seasonal affective disorder (SAD), which causes depression-like symptoms such as low mood, fatigue, and irritability. Since menopause already affects mood regulation, the winter season can deepen feelings of anxiety, sadness, and exhaustion.
Vitamin D deficiency is particularly important because it plays a crucial role in bone health, immune function, and mood stabilization. With less sun exposure in winter, vitamin D levels drop, worsening bone density loss and increasing the risk of osteoporosis, a concern already heightened by menopause.
In summary, the interplay of hormonal changes with environmental and lifestyle factors in winter—such as temperature fluctuations, dry air, reduced sunlight, and cold weather—makes menopause symptoms like hot flashes, joint pain, skin dryness, sleep problems, and mood disturbances feel more intense and harder to manage during the colder months.