Chemotherapy can indeed cause early menopause, often referred to as chemotherapy-induced menopause. This happens because chemotherapy drugs, which are designed to kill rapidly dividing cancer cells, can also affect the ovaries, which contain eggs and produce hormones like estrogen and progesterone. When the ovaries are damaged by chemotherapy, their function can decline or stop altogether, leading to a reduction or cessation of hormone production and the onset of menopause symptoms earlier than the natural age of menopause.
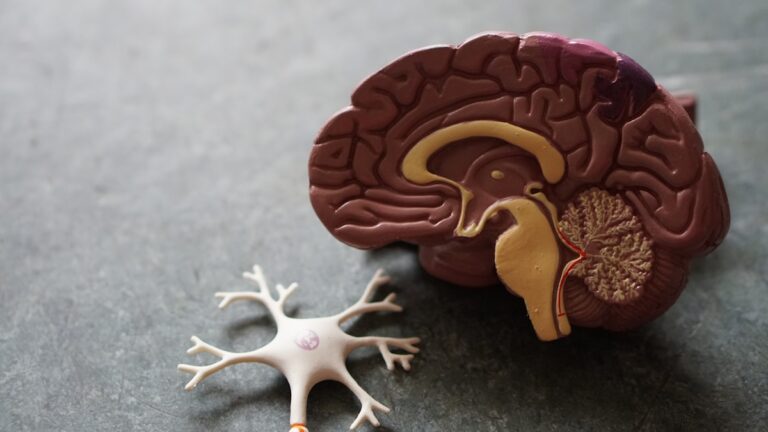
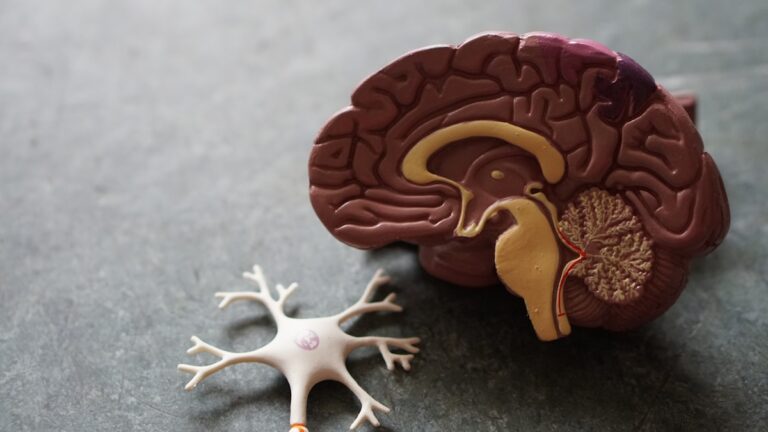
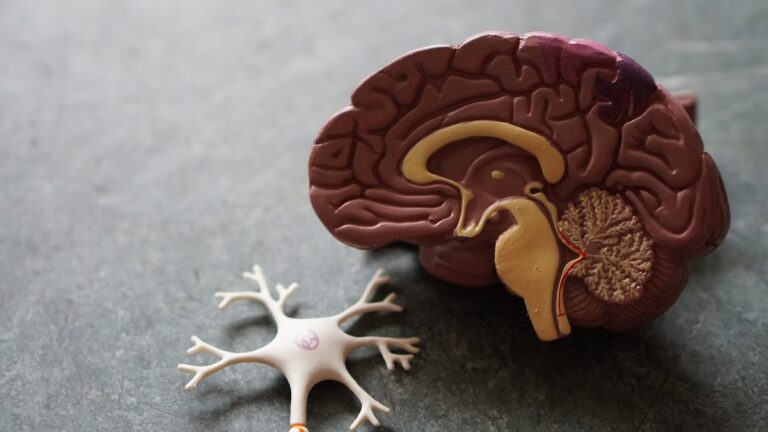
The process by which chemotherapy causes early menopause involves its impact on the hypothalamic-pituitary-ovarian (HPO) axis, a complex hormonal signaling system that regulates the menstrual cycle. Chemotherapy can disrupt this axis, either temporarily or permanently, by damaging ovarian follicles or interfering with hormone signaling. The extent of ovarian damage depends on several factors, including the type and dose of chemotherapy drugs used, the duration of treatment, and the age of the woman at the time of treatment. Younger women tend to have a larger reserve of ovarian follicles and may recover ovarian function after chemotherapy, while older women are more likely to experience permanent menopause because their ovarian reserve is already diminished.
Symptoms of chemotherapy-induced early menopause can appear suddenly or gradually and often mirror those of natural menopause. These include hot flashes, night sweats, mood swings, vaginal dryness, irregular or stopped periods, and sleep disturbances. Some women may also experience joint aches and decreased libido. The severity of symptoms varies widely among individuals. For some, chemotherapy-induced menopause is temporary, and menstruation may resume months or years after treatment ends. For others, especially if the ovaries are severely damaged or removed surgically, menopause is permanent.
Certain cancer treatments beyond chemotherapy can also contribute to early menopause. Radiation therapy, especially when targeted near the pelvic area, can damage the ovaries and reduce hormone production. Surgical procedures, such as the removal of ovaries (oophorectomy) or the uterus (hysterectomy), can induce menopause either immediately or over time depending on whether the ovaries remain intact. Additionally, hormone therapies used in cancers like breast cancer, such as aromatase inhibitors or tamoxifen, can cause menopausal symptoms by lowering estrogen levels, even if the ovaries are still functioning.
Managing early menopause caused by chemotherapy involves addressing both the symptoms and the long-term health effects of reduced estrogen. Hormone replacement therapy (HRT) is often effective in relieving symptoms like hot flashes and vaginal dryness, but its use must be carefully considered, especially in women with hormone-sensitive cancers. Non-hormonal treatments, lifestyle changes, and supportive therapies can also help manage symptoms. For women concerned about fertility, options like egg or embryo freezing before starting chemotherapy are important to discuss with healthcare providers, as chemotherapy can impair fertility by damaging ovarian function.
In summary, chemotherapy can cause early menopause by damaging the ovaries and disrupting hormonal cycles. The onset and permanence of menopause depend on individual factors such as age, type of chemotherapy, and additional treatments. Symptoms can be intense and sudden, but there are ways to manage them and support overall health during and after cancer treatment.