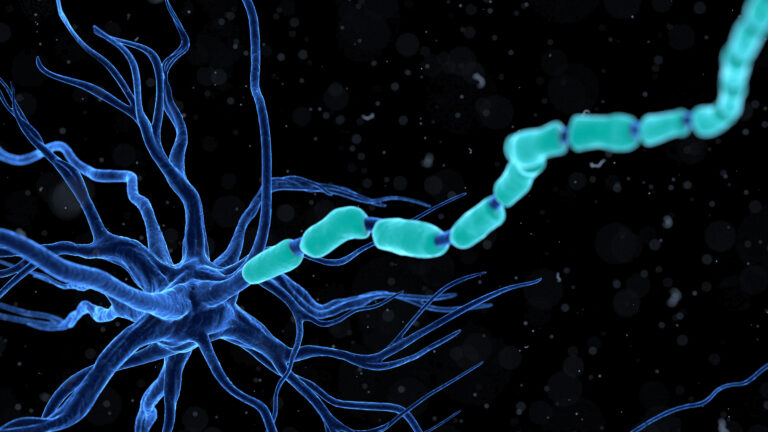
Shingles flare-ups happen when the varicella-zoster virus, which causes chickenpox, reactivates in the body after lying dormant for years. This virus hides in nerve cells near the spinal cord or brain after a person recovers from chickenpox. When the virus wakes up, it travels along nerve fibers to the skin, causing the painful rash and other symptoms associated with shingles.
Several factors can trigger this reactivation, leading to shingles flare-ups. The most common cause is a weakened immune system. As people age, their immune defenses naturally decline, making it easier for the virus to reactivate. Stress is another major trigger because it can suppress the immune system, reducing the body’s ability to keep the virus in check. Physical or emotional stress, illness, or trauma can all contribute to this immune suppression.
Certain medical conditions that impair immunity, such as HIV/AIDS, cancer, or autoimmune diseases, increase the risk of shingles flare-ups. Treatments that weaken the immune system, like chemotherapy, radiation, or long-term use of steroids and immunosuppressive drugs, also raise the chances of the virus reactivating.
Other triggers include nerve damage or injury, which can disturb the nerves where the virus resides, potentially prompting it to reactivate. Even something like surgery or a severe sunburn on a specific area of the body might provoke a flare-up in that region.
The early signs of a shingles flare-up often include pain, tingling, burning, or stabbing sensations localized to one side of the body or face. This nerve pain can be intense and may occur before any visible rash appears. After a couple of days, a rash develops in the affected area, starting as red or discolored patches that quickly turn into fluid-filled blisters. These blisters eventually break open, crust over, and heal, but the pain can persist long after the rash disappears.
In some cases, the nerve pain continues for months or even years after the rash has healed, a condition known as postherpetic neuralgia. This happens because the virus damages the nerves during the flare-up, causing ongoing pain signals even when the skin looks normal.
Certain lifestyle factors can influence the likelihood of shingles flare-ups. Poor nutrition, lack of sleep, and chronic stress can all weaken the immune system. Gut health may also play a role; imbalances in gut bacteria (gut dysbiosis) can affect immune function and potentially trigger flare-ups.
In summary, shingles flare-ups are caused by the reactivation of the dormant varicella-zoster virus, primarily due to weakened immunity from aging, stress, illness, or medical treatments. Nerve injury and lifestyle factors can also contribute. The flare-up process involves nerve pain followed by a characteristic rash and sometimes long-lasting nerve pain after the rash heals. Managing stress, maintaining a healthy immune system, and early medical treatment can help reduce the severity and frequency of shingles flare-ups.