Headaches are one of the most common health complaints worldwide, affecting people of all ages and backgrounds. Understanding why you have a headache involves exploring a complex interplay of neurological, vascular, genetic, environmental, and lifestyle factors. The causes can range from simple, temporary triggers to chronic neurological disorders.
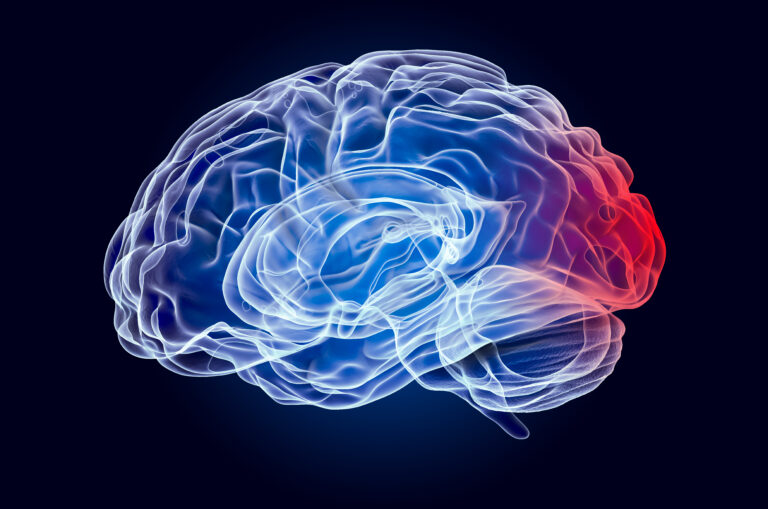
At the core, headaches arise from the activation or irritation of pain-sensitive structures in the head, including nerves, blood vessels, muscles, and tissues surrounding the brain. Contrary to older beliefs that headaches, especially migraines, were primarily caused by blood vessel abnormalities, modern research has shifted the understanding toward neurological origins. For example, migraines are now recognized as a neurological disorder involving complex brain signaling rather than just vascular changes[1][2].
One key discovery in headache science is the role of a neurotransmitter called **calcitonin gene-related peptide (CGRP)**. CGRP is released from nerve endings around blood vessels and contributes to migraine symptoms by promoting inflammation and pain signaling. This insight has led to new treatments targeting CGRP to reduce migraine frequency and severity[1]. However, these treatments only provide permanent relief for about 20% of patients, highlighting the complexity of headache disorders and the need for personalized approaches[1].
**Types of Headaches and Their Causes**
1. **Migraine Headaches**
Migraines are severe, throbbing headaches often localized to one side of the head, sometimes accompanied by nausea, sensitivity to light and sound, and neurological symptoms called aura. The aura can include visual disturbances, sensory changes, or speech difficulties caused by waves of electrical or chemical activity spreading across the brain, a phenomenon known as *cortical spreading depression*[3].
Migraines are influenced by genetic predisposition, hormonal fluctuations (especially in women), environmental triggers (such as bright lights, strong odors, or certain foods), and lifestyle factors like stress and sleep patterns[2][3]. Hormonal changes during menstruation are a common trigger for many women, explaining the higher prevalence of migraines in females[2][3].
2. **Tension-Type Headaches (TTH)**
These are the most common headaches, characterized by a dull, pressing pain often described as a tight band around the head. TTH is usually related to muscle tension, stress, anxiety, or poor posture. Although less severe than migraines, chronic tension headaches can significantly impair quality of life, causing emotional distress and social dysfunction[4].
3. **Cluster Headaches**
Cluster headaches are rare but extremely painful headaches that occur in cyclical patterns or clusters. They involve intense pain around one eye, often accompanied by autonomic symptoms like tearing, nasal congestion, or eyelid drooping. Cluster headaches are now understood as neurological disorders with distinct clinical profiles and require specialized management[4].
4. **Secondary Headaches**
These headaches result from underlying medical conditions such as infections, head injuries, sinus problems, or medication overuse. Identifying and treating the root cause is essential in these cases.
**Why Do Headaches Occur?**
– **Neurological Mechanisms:** Modern science shows that headaches, especially migraines, involve abnormal brain activity and neurotransmitter imbalances. The release of CGRP and other chemicals causes inflammation and sensitization of pain pathways[1][2].
– **Genetics:** Family history plays a significant role, with certain genes linked to increased susceptibility to migraines[2][3].
– **Hormonal Influences:** Fluctuations in estrogen and other hormones can trigger headaches, explaining why women are more affected[2][3].
– **Environmental and Lifestyle Triggers:** Stress, lack of sleep, certain foods (like those containing MSG or excessive caffeine), alcohol, bright lights, and strong odors can provoke headaches[3].
– **Psychological Factors:** Anxiety, depression, and chronic stress can exacerbate headache frequency and intensity[4].
**Complications and Impact**
Headaches, particularly migraines, can severely affect daily functioning and quality of life. They are associated with poor sleep, emotional distress, and increased risk of mental health disorders such as anxiety and depression[4]. People with migraine with aura have a slightly increased risk of stroke, underscoring the importance of medical evaluation and management[3].
**Treatment and Management**
Treatment depends on the headache type and severity. For migraines, medications targeting CGRP and other neurotransmitters have revolutionized care but are not universally effective[1]. Lifestyle modifications, stress management, and avoiding known triggers are critical components of headache prevention[3]. Overuse of pain medications can lead to medication overuse headaches, a condition where frequent use of headache drugs paradoxically causes more headaches[3].
Healthcare providers emphasize the importance of patient-reported outcomes to tailor treatments and improve quality of life. Ongoing research aims to better understand headache mechanisms and develop more effective therapies[4].
—
**Sources:**
[1] MIT News, “A better understanding of debilitating head pain,” 2025
[2] EBSCO Research Starters, “Migraine headaches”
[3] Mayo Clinic, “Migraine with aura – Symptoms & causes,” 2025
[4] Healthcare Bulletin, “Study of Clinical Profile of Primary Headache Disorders and Its Effect on Quality of Life,” 2025