Rivastigmine capsules, used primarily to treat symptoms of Alzheimer’s disease and other dementias, can cause a variety of side effects that range from mild to severe. The most frequently reported side effects are related to the digestive system. Patients often experience nausea and vomiting, especially during the initial phase when the dose is gradually increased. This happens because rivastigmine affects enzymes in the brain but also influences parts of the body involved in digestion. Taking the medication with food and increasing doses slowly can help reduce these uncomfortable symptoms.
Loss of appetite is another common issue, which sometimes leads to weight loss over time. Diarrhea and stomach pain or upset are also reported by many users. These gastrointestinal problems tend to be more prominent at higher doses or when treatment begins but may lessen as the body adjusts.
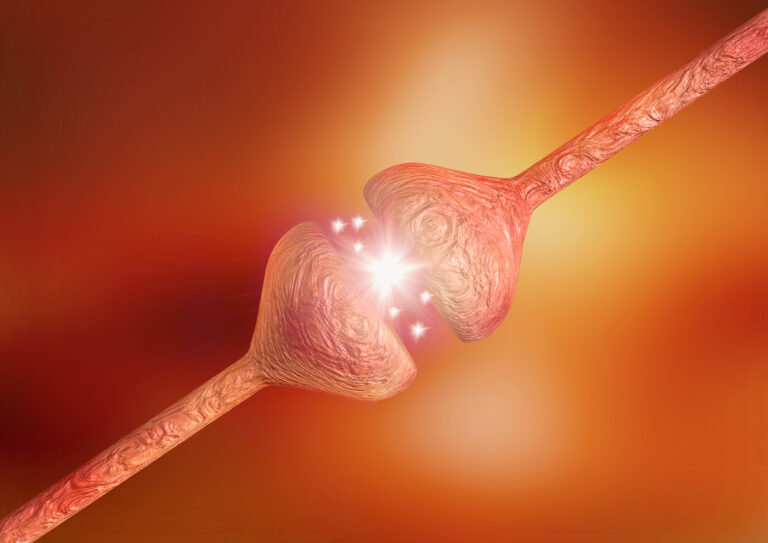
Beyond digestive troubles, some people taking rivastigmine capsules notice dizziness or headaches. These neurological side effects occur because rivastigmine acts on neurotransmitters in the brain that regulate various functions including balance and pain perception.
Muscle-related symptoms such as tremors (shaking), cramps, weakness, or fatigue have been observed too. These may be linked to how rivastigmine influences nerve signals controlling muscle activity.
Sleep disturbances like insomnia or unusual dreams can happen but are less common than other side effects.
In rare cases, serious adverse reactions require immediate medical attention:
– Severe vomiting leading to dehydration
– Slow heart rate (bradycardia), which might cause fainting or chest discomfort
– Allergic reactions presenting as rash, itching, swelling (especially around face or throat), difficulty breathing
– Angioedema—a sudden swelling beneath the skin—though very uncommon
Because rivastigmine increases acetylcholine levels by inhibiting cholinesterase enzymes in both central nervous system and peripheral tissues, it can affect multiple organ systems beyond just cognition improvement.
Some patients using transdermal patches instead of capsules report fewer gastrointestinal issues like nausea but may develop skin irritation such as redness, itching, vesicles (small blisters), or swelling at patch sites due to allergic contact dermatitis.
Long-term use has been associated with an increased risk of mortality compared with some alternative treatments for dementia; however this finding requires careful interpretation within clinical context since underlying disease severity varies among patients treated with different drugs.
Precautions before starting rivastigmine include informing your healthcare provider if you have liver problems since metabolism might be affected; kidney issues; heart conditions like arrhythmias; asthma; history of stomach ulcers; low body weight which could increase sensitivity; pregnancy or breastfeeding status since safety data is limited there.
Patients should never stop taking rivastigmine suddenly without consulting their doctor because abrupt discontinuation might worsen cognitive symptoms abruptly rather than gradually improving them over time through proper dosing adjustments.
Regular monitoring during therapy involves checking cognitive function progress alongside physical health markers such as weight changes due to appetite loss and hydration status if vomiting occurs frequently enough for concern about dehydration risk.
In summary — while rivastigmine capsules offer benefits for managing dementia-related memory loss and behavioral difficulties — they come with a spectrum of possible side effects mostly centered on gastrointestinal discomforts plus occasional neurological complaints like dizziness and tremors along with rare serious risks requiring urgent care attention. Proper dosing strategies including slow titration schedules combined with food intake help minimize many adverse events making treatment more tolerable for patients living with cognitive decline disorders.