**The Intersection of Vascular Health and Alzheimer’s: Understanding Cognitive Decline**
Alzheimer’s disease and vascular health are two interconnected factors that significantly impact cognitive decline. While Alzheimer’s is often associated with amyloid buildup in the brain, vascular health plays a crucial role in maintaining brain function. Here, we explore the scientific perspectives on how vascular health intersects with Alzheimer’s, leading to cognitive impairment.
### Blood Vessel Dysfunction and Memory Loss
Recent studies have highlighted the importance of blood vessel health in the brain, particularly in the temporal lobes, which are responsible for memory. A study led by the University of Southern California (USC) found that mild cognitive impairment is linked to blood vessel dysfunction in the temporal lobes. This dysfunction can lead to memory problems, even in individuals without amyloid buildup in the brain[1].
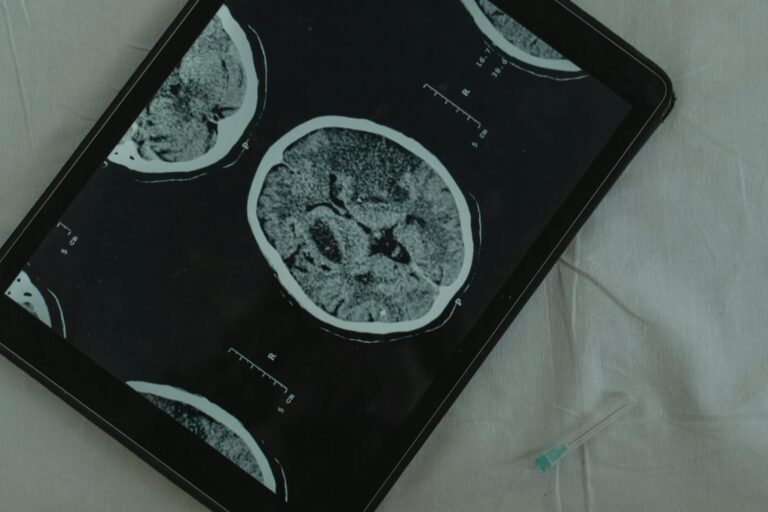
Researchers used magnetic resonance imaging (MRI) to observe how well the brain’s blood vessels dilated in response to stimuli. Participants who showed poor dilation in their blood vessels exhibited signs of cognitive impairment. This suggests that blood vessel health is a critical factor in memory decline, and focusing on vascular health could provide new insights into diagnosing and treating dementia.
### Traditional Risk Factors Reevaluated
Traditionally, high blood pressure and diabetes have been known to damage brain blood vessels, increasing the risk of cognitive decline. However, a study by the University of California, Irvine, challenged these traditional risk factors by examining individuals over 90 years old. The study found that these patterns may change with age, and even more intriguingly, the use of blood pressure-lowering medication in this age group was linked to a lower likelihood of specific types of brain damage[2].
### Vascular Disorders and Alzheimer’s Disparity
Vascular disorders, such as hypertension and cardiovascular disease, are strong risk factors for Alzheimer’s disease and related dementias (ADRD). A multiethnic cohort study found that controlling for vascular disorders mediated the AD health disparity observed across racial/ethnic groups. This suggests that vascular health has a significant influence on cognitive functions and neurodegeneration across different populations[3].
### Glymphatic System and Waste Clearance
Another critical aspect of vascular health is the glymphatic system, which helps clear waste from the brain. Vascular dementia, the second most common form of dementia after Alzheimer’s, is often caused by cerebral small vessel disease (cSVD), which damages the brain’s small blood vessels. Researchers from the Keck School of Medicine of USC have found new evidence linking cSVD to problems with the glymphatic system. They used a technique called Diffusion Tensor Image Analysis along the Perivascular Space (DTI-ALPS) to determine how well the glymphatic system was functioning in each person based on their brain scans. The study confirmed that a low DTI-ALPS score is a biomarker for cSVD and suggests that glymphatic damage may be driving cognitive decline[4].
### Conclusion
The intersection of vascular health and Alzheimer’s disease is complex and multifaceted. While amyloid buildup is a significant factor in Alzheimer’s, vascular health plays a crucial role in maintaining brain function. Blood vessel dysfunction, glymphatic system problems, and vascular disorders all contribute to cognitive decline. By focusing on vascular health, researchers and clinicians can develop new diagnostic approaches and treatments for dementia, potentially improving outcomes for individuals affected by these conditions.
In summary, understanding the relationship between vascular health and Alzheimer’s disease is essential for addressing cognitive decline. By integrating vascular health into diagnostic and therapeutic strategies, we can better manage and prevent the progression of dementia.