Pharmacogenomics is a relatively new field in medicine that combines the study of genetics and pharmacology. It focuses on how an individual’s genes affect their response to medications, specifically in the treatment of diseases and disorders. One area of medicine where this field is making significant strides is in the treatment of Alzheimer’s disease.
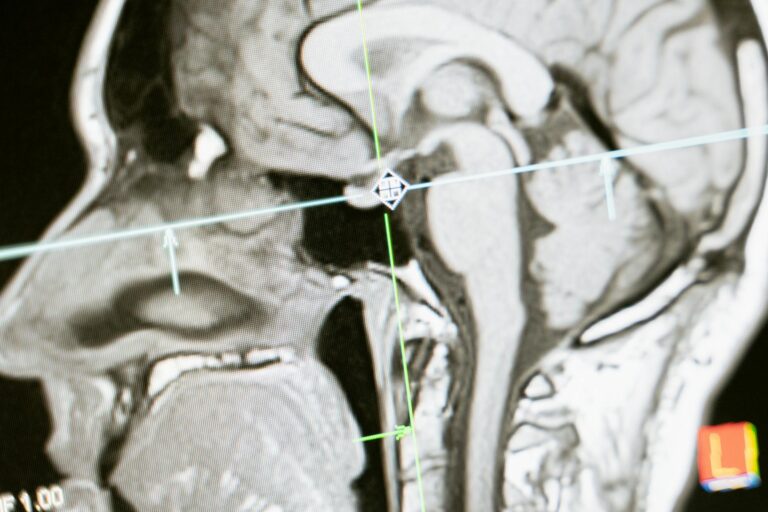
Alzheimer’s disease is a progressive disorder that affects the brain, leading to memory loss, cognitive decline, and behavioral changes. It is the most common form of dementia and affects millions of people worldwide. Although there is currently no cure for Alzheimer’s disease, there are medications that can help improve symptoms and slow down the progression of the disease. However, not all patients respond to these medications in the same way, and this is where pharmacogenomics comes into play.
Pharmacogenomics in Alzheimer’s treatment involves analyzing an individual’s genetic makeup to determine which medications are most likely to be effective and which may cause adverse effects. The variation in genes among individuals can affect how they metabolize and respond to certain medications. By understanding these genetic differences, doctors can personalize treatment plans for each patient, leading to more effective and safer treatment options.
One of the main medications used in the treatment of Alzheimer’s disease is cholinesterase inhibitors. These drugs work by increasing the levels of a chemical called acetylcholine in the brain, which is responsible for memory and learning. However, studies have shown that some patients with specific genetic variations do not respond well to cholinesterase inhibitors and may even experience adverse effects. By using pharmacogenomics, doctors can identify these individuals before prescribing the medication, reducing the risk of side effects and improving treatment outcomes.
Another medication commonly used in Alzheimer’s treatment is memantine, which works by regulating the activity of another chemical called glutamate. Similar to cholinesterase inhibitors, studies have shown that certain genetic variations can affect how patients respond to memantine. By using pharmacogenomics, doctors can determine the most effective dosage for each patient, leading to better treatment outcomes.
In addition to improving the effectiveness and safety of current Alzheimer’s medications, pharmacogenomics is also playing a role in the development of new treatments. With a better understanding of how genetic variations affect drug response, researchers can develop more targeted and personalized medications for Alzheimer’s disease. This not only increases the chances of success but also reduces the risk of adverse effects.
Furthermore, pharmacogenomics is not only limited to medication-based treatments. It also plays a significant role in non-pharmacological therapies for Alzheimer’s, such as lifestyle interventions and dietary changes. For example, studies have shown that certain genetic variations can affect how individuals respond to a Mediterranean diet, which has been linked to a reduced risk of developing Alzheimer’s disease. By using pharmacogenomics, doctors can identify individuals who may benefit the most from this dietary approach and tailor recommendations accordingly.
However, despite the potential benefits of pharmacogenomics in Alzheimer’s treatment, there are still some challenges to overcome. One of the main challenges is access to genetic testing. While genetic testing is becoming more widely available, it can still be costly and not covered by insurance. There is also a lack of standardized guidelines for incorporating pharmacogenomics into clinical practice. As a result, many doctors may not be familiar with or have access to the necessary tools and resources to utilize this technology.
In conclusion, pharmacogenomics is a promising field that is revolutionizing the treatment of Alzheimer’s disease. By understanding how an individual’s genes affect their response to medication, doctors can personalize treatment plans, leading to better outcomes and reduced risk of adverse effects. However, there is still a need for more research and education in this area to make it more accessible and widely implemented in clinical practice. With continued advancements in technology and increased awareness, pharmacogenomics has the potential to greatly improve the lives of those living with Alzheimer’s disease.