Alzheimer’s disease is a progressive neurodegenerative disorder that affects millions of people worldwide. It is the most common form of dementia, accounting for about 60-80% of all dementia cases. This disease primarily affects the elderly population, with most cases occurring after the age of 65. It is characterized by memory loss, cognitive decline, and behavioral changes that interfere with daily activities. The pathophysiology of Alzheimer’s disease is complex and not yet fully understood, but research has identified several key factors that contribute to its development.
To understand the pathophysiology of Alzheimer’s disease, we first need to understand the structure and function of the brain. The brain is made up of billions of neurons, which are nerve cells responsible for transmitting information through electrical and chemical signals. These neurons are supported by glial cells, which provide structural and functional support to the brain. The communication between neurons is crucial for all brain functions, including memory, thinking, and problem-solving.
In Alzheimer’s disease, there is a progressive loss of neurons and their connections (synapses) in specific regions of the brain. This loss is caused by the accumulation of abnormal protein deposits in the brain, leading to nerve cell death and brain shrinkage. These protein deposits include beta-amyloid plaques and tau tangles.
Beta-amyloid plaques are formed when a protein called amyloid precursor protein (APP) is broken down into smaller fragments, one of which is beta-amyloid. Normally, these fragments are cleared by the body’s immune system, but in Alzheimer’s disease, they accumulate and form sticky clumps outside of neurons. These plaques interfere with the communication between neurons, leading to their dysfunction and eventual death.
Tau tangles are formed when another protein called tau becomes abnormal and clumps together inside neurons. Tau is an essential protein for maintaining the structure and transport system within neurons. In Alzheimer’s disease, tau tangles disrupt this system and cause the neurons to die.
The exact cause of the accumulation of these protein deposits is still unknown, but researchers believe that a combination of genetic and environmental factors may play a role. Genetic mutations in certain genes, such as the amyloid precursor protein (APP) gene, have been linked to the development of Alzheimer’s disease. However, these mutations are rare, and most cases of Alzheimer’s disease are thought to be caused by a combination of genetic and environmental factors.
One of the key mechanisms involved in the pathophysiology of Alzheimer’s disease is inflammation. Inflammation is the body’s natural response to injury or infection, and it is essential for healing. However, in Alzheimer’s disease, chronic inflammation occurs in the brain, which contributes to nerve cell death and damage. This inflammation is caused by the activation of immune cells called microglia, which release toxic substances that can damage neurons.
Another factor that contributes to the pathophysiology of Alzheimer’s disease is oxidative stress. Oxidative stress occurs when there is an imbalance between the production of harmful free radicals and the body’s ability to neutralize them. Free radicals can damage cells, including neurons, and contribute to their death. In Alzheimer’s disease, there is evidence of increased oxidative stress in the brain, which can further exacerbate nerve cell damage.
Furthermore, research has also shown that there are changes in the brain’s energy metabolism in Alzheimer’s disease. The brain requires a constant supply of glucose to function correctly, but in this disease, there is a significant decrease in glucose utilization. This can result in reduced energy production and contribute to the malfunctioning and death of neurons.
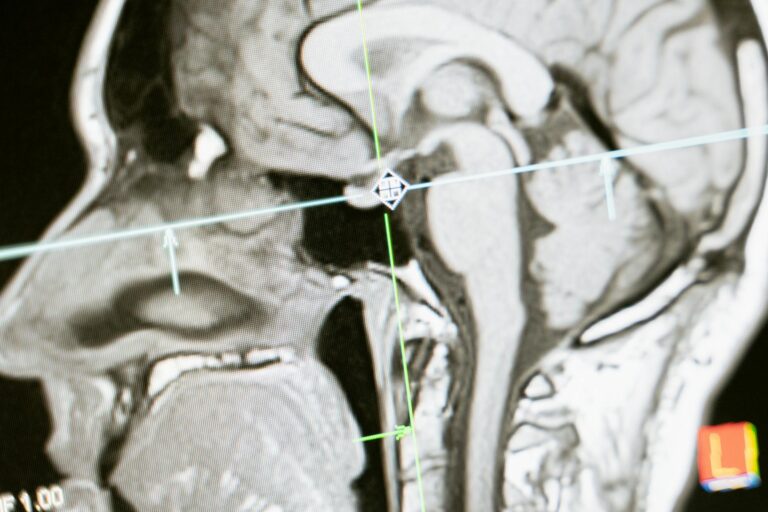
As the disease progresses, the loss of neurons and their connections leads to significant changes in the brain’s structure. These changes can be seen on brain imaging scans, such as magnetic resonance imaging (MRI) and positron emission tomography (PET) scans. The brain shrinks as the disease progresses, and there is a significant decrease in the size of the hippocampus, a region of the brain responsible for memory.
In conclusion, the pathophysiology of Alzheimer’s disease is a complex process involving various factors such as the accumulation of abnormal protein deposits, inflammation, oxidative stress, and changes in energy metabolism. These factors contribute to the progressive loss of neurons and their connections, leading to the characteristic symptoms of memory loss, cognitive decline, and behavioral changes. Although there is still much to learn about this disease, understanding its pathophysiology is crucial in developing effective treatments and ultimately finding a cure.