### Beyond the Plaque: Hidden Pathways in Neurodegeneration
Alzheimer’s disease is often associated with two main culprits: amyloid plaques and neurofibrillary tangles. These abnormal structures in the brain are thought to contribute to the loss of memory and cognitive function. However, recent research suggests that there are more complex and interconnected pathways at play in neurodegeneration.
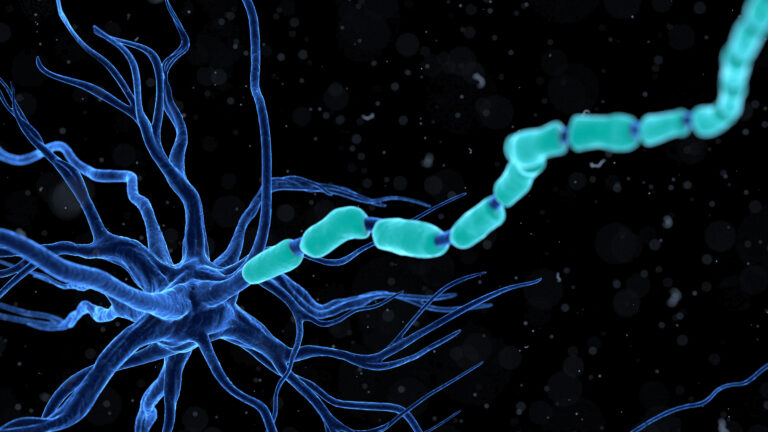
#### The Role of Microglia
Microglia are the brain’s immune cells, responsible for cleaning up debris and protecting neurons. In Alzheimer’s disease, microglia can become dysfunctional, leading to increased inflammation and further damage to brain cells. This inflammation can exacerbate the formation of amyloid plaques and tau tangles, creating a vicious cycle of neurodegeneration.
#### The Impact of Head Trauma
Head trauma, such as concussions, can reactivate dormant viruses like herpes simplex virus type 1 (HSV-1) in the brain. This reactivation can trigger a cascade of damage associated with Alzheimer’s disease, including the formation of amyloid plaques and tau tangles. The study using 3D bioengineered human brain tissue models showed that mechanical disruptions, simulating concussions, reactivated HSV-1, leading to widespread inflammation and neurodegenerative markers characteristic of Alzheimer’s disease[2].
#### Epigenetic Changes
Epigenetics, the study of gene expression changes without altering the DNA sequence, plays a significant role in Alzheimer’s disease. Environmental factors and lifestyle choices can influence epigenetic changes, which in turn affect gene expression patterns. These changes can contribute to the dysregulation of crucial cellular processes, including synaptic plasticity, neuroinflammation, and oxidative stress. This dynamic interplay between genetic and environmental factors influences the epigenetic landscape in AD, altering gene expression patterns and key pathologic events associated with disease pathogenesis[3].
#### Interactions Between Neurodegenerative Diseases
Different neurodegenerative diseases, such as Alzheimer’s, Lewy Body Dementia, and Vascular Contributions to Cognitive Impairment and Dementia, often co-occur in individuals. These co-occurring pathologies complicate both pathophysiological investigation and treatment development. Research is needed to understand how different neurodegenerative diseases interact clinically and physiologically. Identifying which neurodegenerative processes are active in individuals and how they resemble and differ from one another at the molecular, cellular, and organismic levels is crucial for developing effective treatments[1].
#### New Directions in Research
The traditional focus on amyloid plaques and tau tangles has led to some promising but limited treatments. New research is exploring the critical role of microglia in Alzheimer’s disease, suggesting that targeting microglial dysfunction could be a more effective approach. Additionally, understanding the mechanisms by which head trauma and viral reactivation contribute to neurodegeneration offers new avenues for intervention, such as antiviral and anti-inflammatory treatments.
In summary, while amyloid plaques and tau tangles are well-known markers of Alzheimer’s disease, the complexity of neurodegeneration involves multiple hidden pathways. Understanding these pathways, including the role of microglia, the impact of head trauma, and epigenetic changes, is essential for developing more effective treatments and preventing the progression of neurodegenerative diseases.