Ativan, the brand name for lorazepam, is a benzodiazepine medication sometimes used to manage anxiety, agitation, or acute behavioral disturbances in patients with Alzheimer’s disease or other dementias. However, its safety profile in Alzheimer’s patients is complex and generally warrants caution due to potential risks and side effects.
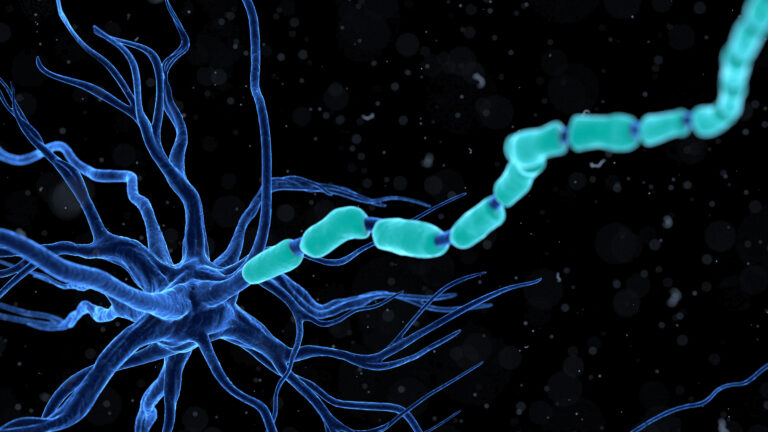
Benzodiazepines like Ativan act by enhancing the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that produces calming effects on the brain. While this can temporarily reduce anxiety or agitation, benzodiazepines are associated with several adverse effects in older adults, especially those with cognitive impairment such as Alzheimer’s disease.
One major concern is that benzodiazepines may **accelerate cognitive decline** and worsen dementia symptoms. They can increase confusion, sedation, and the risk of falls, which are particularly dangerous in elderly patients with Alzheimer’s. Long-term use has also been linked to an increased risk of developing dementia in the first place, according to some evidence[5].
In acute situations where a patient with dementia is physically aggressive or poses a danger to themselves or others, short-term use of lorazepam may be considered. For example, intramuscular lorazepam can be used to quickly calm severe agitation or aggression, especially if benzodiazepine withdrawal is suspected. However, haloperidol, an antipsychotic, is often preferred because it tends to cause less drowsiness and cognitive impairment than lorazepam in these patients[4].
Clinical guidelines generally recommend **avoiding benzodiazepines for routine management of behavioral symptoms in Alzheimer’s patients** due to their side effect profile. They are not considered first-line treatments for agitation or anxiety in dementia. Instead, non-pharmacological approaches and FDA-approved Alzheimer’s medications such as donepezil, rivastigmine, galantamine, and memantine are preferred for managing cognitive symptoms[3].
When benzodiazepines are used, it should be for the shortest duration possible and under close medical supervision. The risk of respiratory problems, pneumonia, and increased sedation must be carefully weighed against the potential benefits[5]. In older adults with dementia, benzodiazepines can cause decreased cognitive performance and worsen sundowning symptoms (evening confusion and agitation)[6].
Recent clinical trials and research emphasize the importance of safety monitoring when using any psychotropic medication in Alzheimer’s patients. For example, studies on other agents like sodium benzoate have shown good tolerability and mild side effects without worsening cognition, highlighting the need for safer alternatives[1].
In summary, Ativan (lorazepam) is **not generally considered safe for routine use in Alzheimer’s patients** due to risks of cognitive worsening, sedation, falls, and other adverse effects. It may be used cautiously and briefly in emergency situations involving severe agitation or aggression but should be avoided for long-term management. Safer, FDA-approved Alzheimer’s medications and non-drug interventions are preferred for managing symptoms in these patients.
Sources:
[1] Academic study on sodium benzoate safety in Alzheimer’s
[3] DailyCaring overview of FDA-approved Alzheimer’s medications
[4] Psychiatric Times on aggression management in dementia
[5] Neural Effects on medications worsening dementia
[6] DrOracle article on benzodiazepines and sundowning in dementia